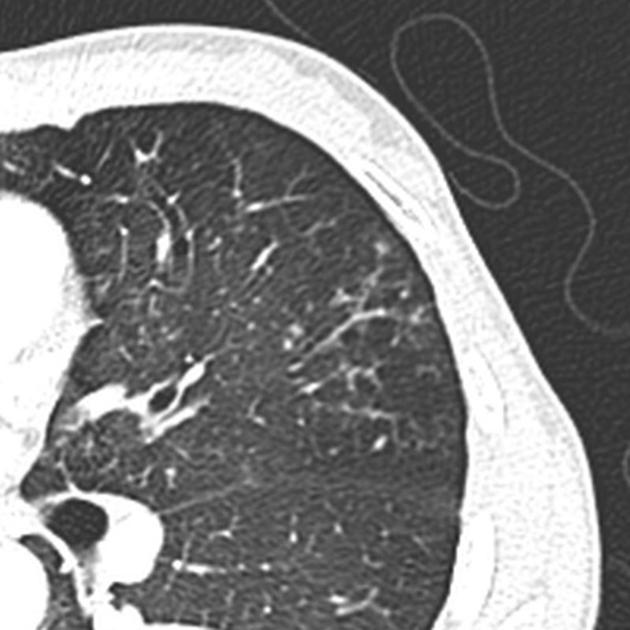
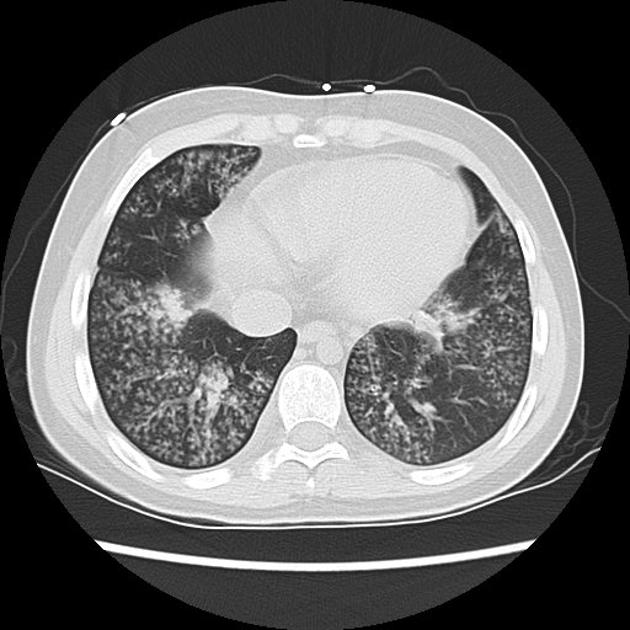
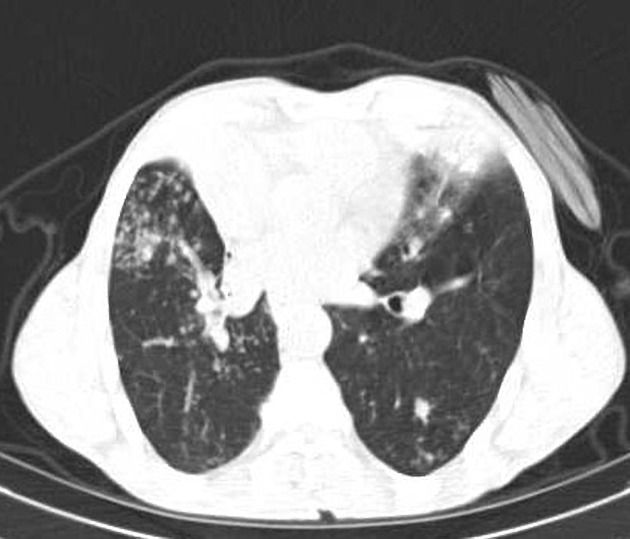
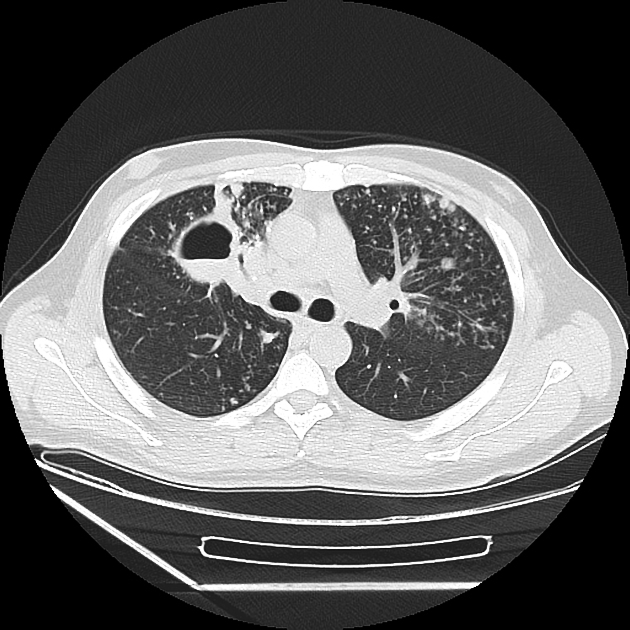
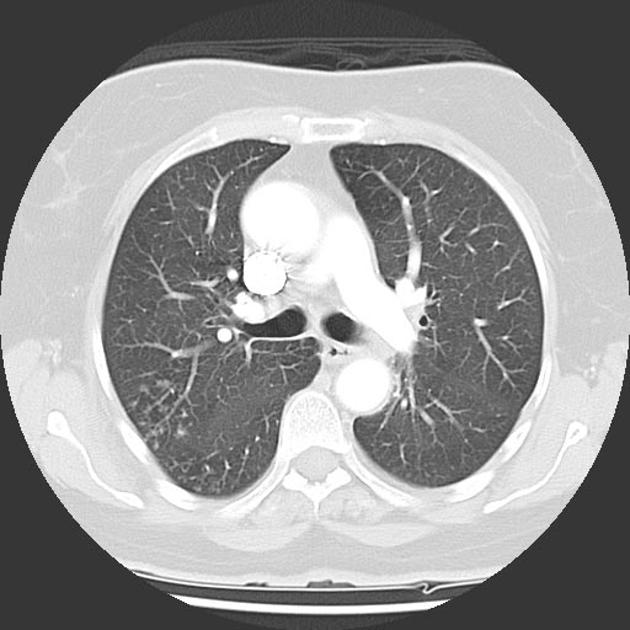
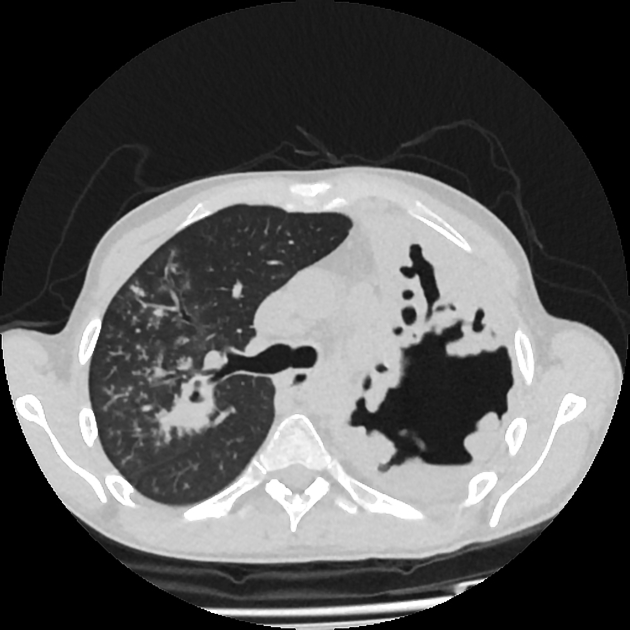
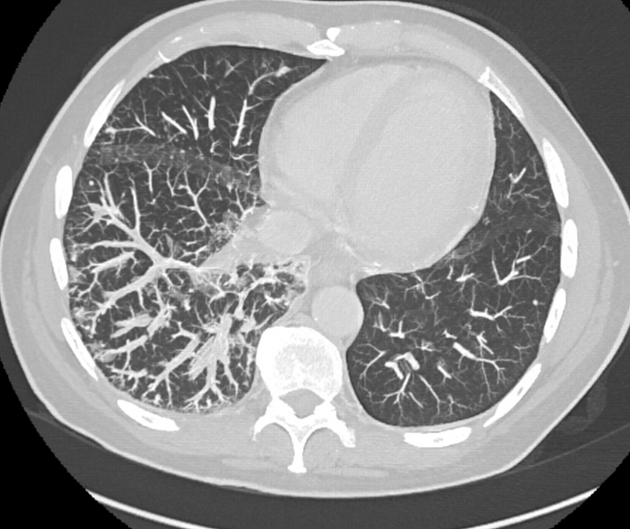
Tree-in-bud pattern describes the CT appearance of multiple areas of centrilobular micronodules with a linear branching pattern, resembling a budding tree 11. Although initially described in patients with endobronchial tuberculosis, it is now recognized in a large number of conditions.
On this page:
Pathology
Simply put, the tree-in-bud pattern can be seen with two main sites of disease 3:
distal airways (more common)
distal pulmonary vasculature
More specifically, the pattern can manifest because of the following disease processes, often in combination:
-
airway-centered
-
bronchioles filled with pus or inflammatory exudate
-
bronchiolitis: thickening of bronchiolar walls and bronchovascular bundle
-
bronchiectasis/bronchiolectasis with mucus plugging
e.g. cystic fibrosis
-
bronchovascular interstitial infiltration
e.g. sarcoidosis, lymphoma, leukemia 4,5
-
-
vascular-centered
-
tumor emboli to centrilobular arteries (or carcinomatous endarteritis)
e.g. breast cancer, stomach cancer
-
granulomatous response to excipient material in intravenous drug users 8,9
e.g. intravenous talcosis or microcrystalline cellulose in crushed oral tablets (excipient lung disease)
-
Etiology
While the tree-in-bud pattern usually represents an endobronchial spread of infection, given the proximity of small pulmonary arteries and small airways (sharing branching morphology in the bronchovascular bundle), a rarer cause of the tree-in-bud pattern is infiltration of the small pulmonary arteries/arterioles or axial interstitium 3,6,7.
Causes include:
-
infective bronchiolitis
-
congenital
-
connective tissue disorders
-
bronchial
-
neoplastic (i.e. carcinomatous endarteritis 3,6,7 or bronchovascular interstitial infiltration 4,5)
distant metastatic disease (e.g. breast, liver, ovary, prostate, kidney)
-
periarterial granulomatous
Radiographic features
The tree-in-bud pattern is not generally visible on plain radiographs 2. It is usually visible on standard CT, however, it is best seen on HRCT chest. Typically the centrilobular nodules are 2-4 mm in diameter and peripheral, within 5 mm of the pleural surface. The connection to opacified or thickened branching structures extends proximally (representing the dilated and opacified bronchioles or inflamed arterioles) 1-3,6.
Practical points
using maximum intensity projection (MIP) can facilitate detection of particularly the centrilobular nodules 6
-
identification of the tree-in-bud pattern should urge you to
look for further imaging findings e.g. thickening of the bronchial wall, narrowing of bronchi, bronchiectasis, consolidation, cavitation, necrotic lymphadenopathy
determine the location (with gravitational or lower lobe predominance favoring aspiration) 6,7
scrutinise patient history, including appropriate exposure history, as this may aid in determining the most likely diagnosis 6,7









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.