Focal nodular hyperplasia (FNH) is a regenerative mass lesion of the liver and the second most common benign liver lesion (the most common is a hemangioma). Many focal nodular hyperplasias have characteristic radiographic features on multimodality imaging, but some lesions may be atypical in appearance. They are typically asymptomatic lesions, usually requiring no treatment.
On this page:
Epidemiology
Focal nodular hyperplasia is most frequently found in young to middle-aged adults, with a strong female predilection 3,4. Around 15% (range 10-20%) of cases occur in men 7. Exogenous estrogens do not cause focal nodular hyperplasia, nor do they cause an increase in size of these masses. Isolated occurrence is the most common but up to 20% of cases may be multiple and can occur with other lesions such as hemangiomas, etc.
Studies since the late 2010s have shown that focal nodular hyperplasia can occur de novo after chemotherapy treatment with oxaliplatin (chemotherapy agent used for bowel and other types of cancer), and less commonly other agents, for example cisplatin and 5-fluorouracil 22,27,28.
Associations
An association with other benign lesions is commonly seen (~25%) 8:
hepatic hemangioma (most common) 6
anomalous venous drainage
hepatic adenoma (possible but not proven) 16
congenital absence of portal vein/portal vein atresia
Clinical presentation
Focal nodular hyperplasias are either found incidentally on imaging or present due to mass effect, with right upper quadrant pain in 20% 5. Unlike hepatic adenomas, complication by spontaneous rupture and hemorrhage is rare 1,4.
Pathology
The origin of focal nodular hyperplasia is thought to be due to a hyperplastic growth of normal hepatocytes with a malformed biliary drainage system, possibly in response to a pre-existent arteriovenous malformation 1,4. The arterial supply is derived from the hepatic artery whereas the venous drainage is into the hepatic veins. Focal nodular hyperplasia does not have a portal venous supply 9.
Focal nodular hyperplasia is divided into two types 4:
typical: 80%
atypical: 20%
Typical focal nodular hyperplasia
Macroscopically, typical lesions demonstrate a mass which is often quite large with well-circumscribed margins but poorly encapsulated. A characteristic feature is a prominent central scar with radiating fibrous septa, but this is present in less than 50% of cases 7. A large central artery is usually present with spoke wheel like centrifugal flow 3,4. Portal veins are absent.
Microscopically, the lesion is composed of abnormal nodular architecture due to fibrous septa radiation from the central scar. There are thick-walled arteries with fibromuscular hyperplasia and abnormal poorly formed elastic lamina in central scar and fibrous septa. An overt ductular reaction is often seen. Nearly normal hepatocytes are arranged in one to two cell-thick plates , architectural and cytologic atypia is absent 26 . Bile ductules are usually found at the interface between hepatocytes and fibrous regions 1,2. Kupffer cells are present 4,7. Immunohistochemistry for glutamine synthetase (GS) has a highly characteristic "map-like pattern" of strong cytoplasmic GS staining in hepatocytes 26 .
There is no malignant potential 1.
Atypical focal nodular hyperplasia
An atypical focal nodular hyperplasia refers to a lesion which lacks the central scar and central artery (making it harder to distinguish from other lesions on gross inspection and imaging), or which demonstrates abnormal nodular architecture and abnormal cholangiolar proliferation 4.
Atypical features also include a pseudocapsule, lesion heterogeneity (more commonly seen in adenoma), non-enhancement of the central scar and intralesional fat 6.
Nodules can grow and disappear, and new nodules can appear even after resection 7.
Variants
Some authors also describe division of atypical focal nodular hyperplasia into several variants which include 8:
telangiectatic variant (also known as an inflammatory hepatic adenoma): most common
mixed hyperplastic and adenomatous variant
lesions with large cell hepatocellular atypia
Radiographic features
As focal nodular hyperplasia is usually treated conservatively, accurate imaging is essential in preventing unnecessary intervention. Moreover, in women of childbearing age, hepatic adenoma is the chief differential diagnosis and biopsy of the latter can result in hemorrhage 1,17.
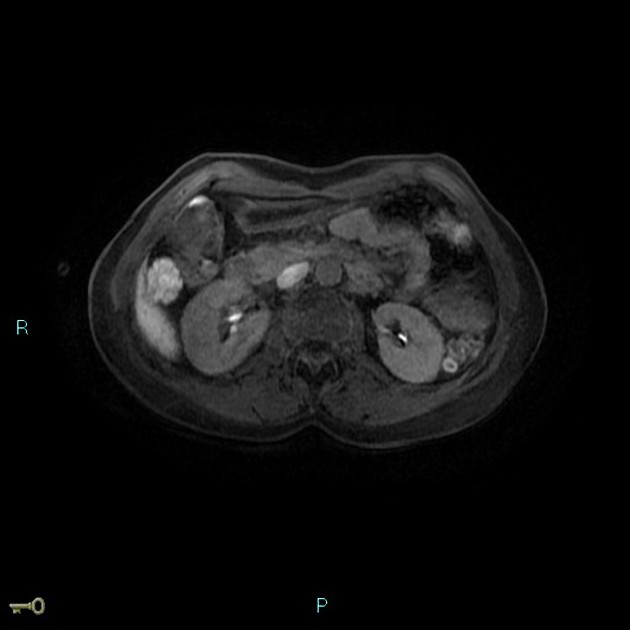
It should be noted that up to 20% of patients with a focal nodular hyperplasia will have multiple lesions 4 and a further 23% will have hemangiomas 4.
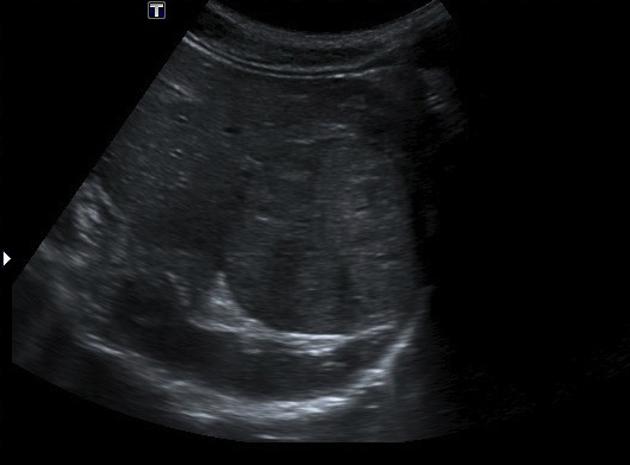
Ultrasound
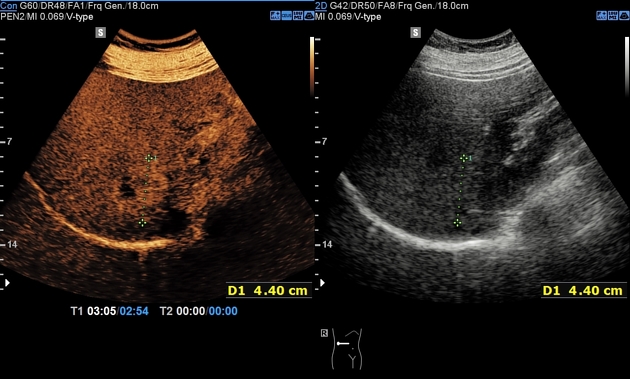
The echogenicity of both focal nodular hyperplasia and its scar is variable, and it may be difficult to detect on ultrasound. Some lesions are well-marginated and easily seen whereas others are isoechoic with surrounding liver. Detectable lesions characteristically demonstrate a central scar with displacement of peripheral vasculature on color Doppler examination. However, these findings are seen in only 20% of cases 4.
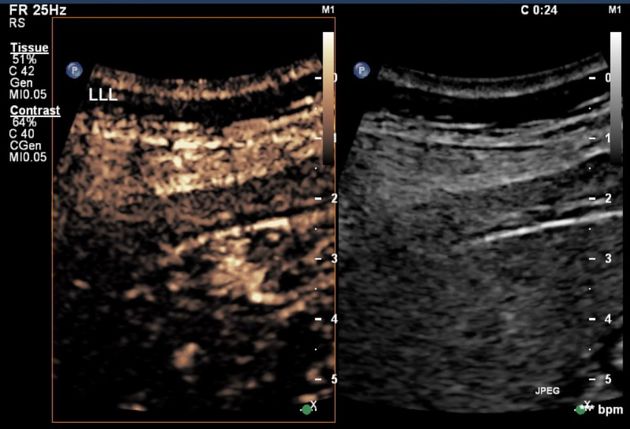
Contrast-enhanced ultrasound
-
early arterial phase 14
focal nodular hyperplasia will enhance relative to background liver
typical focal nodular hyperplasia shows early arterial centrifugal filling (from the center outwards)
prominent feeding vessel may be seen
-
late arterial phase
centrifugal filling (opposite to hemangioma and adenoma)
-
portal venous phase 14
sustained enhancement in the portal venous phase (as opposed to adenoma)
unenhanced scar may be present
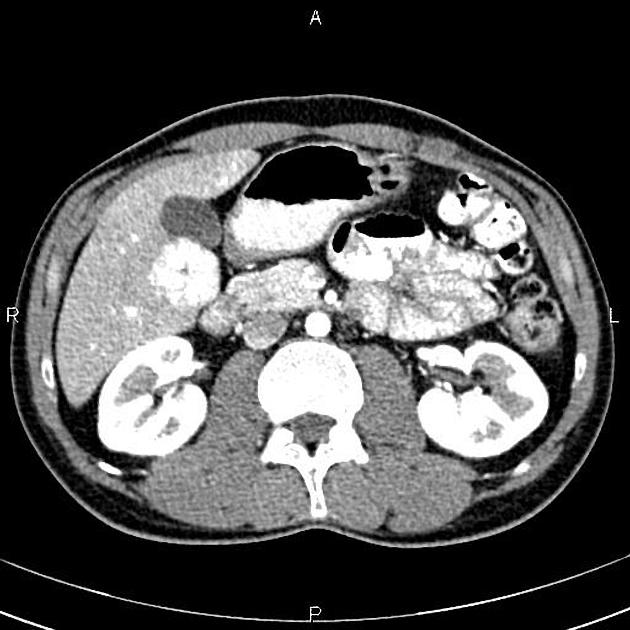
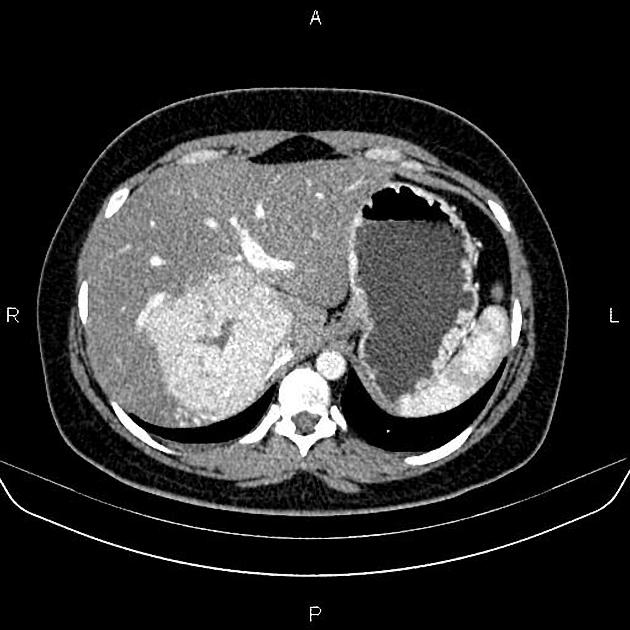
CT
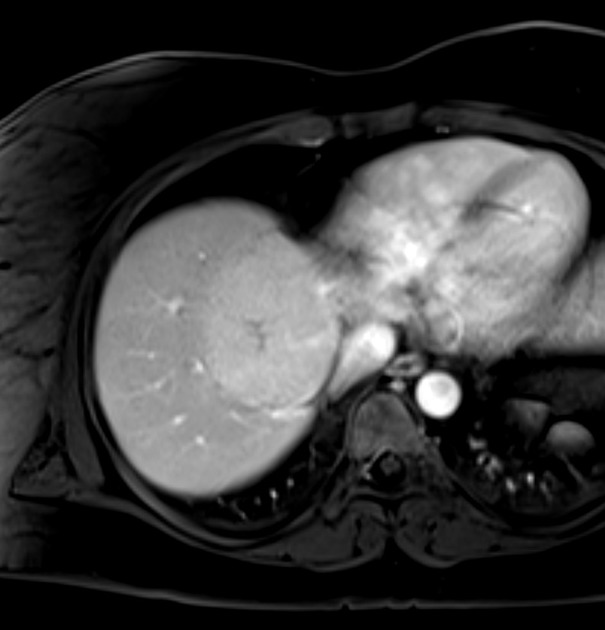
A multiphase liver CT is ideal 4. On the non-contrast series, the lesion is usually hypo- or isoattenuating but may appear hyperattenuating if the rest of the liver is fatty. A hypoattenuating central scar can be seen in up to 60% of lesions >3 cm in size 4.
Focal nodular hyperplasia demonstrates bright homogeneous arterial contrast enhancement except for the central scar which remains hypoattenuating 4. Enlarged central arteries may be seen.
In the portal venous phase, the lesion becomes slightly hyperattenuating or isoattenuating to liver and poorly visualized in many studies, the central scar remains hypodense. Focal nodular hyperplasia is generally not associated with fat, calcification or hemorrhage.
The fibrotic scar demonstrates enhancement on delayed scans in up to 80% of cases 4.
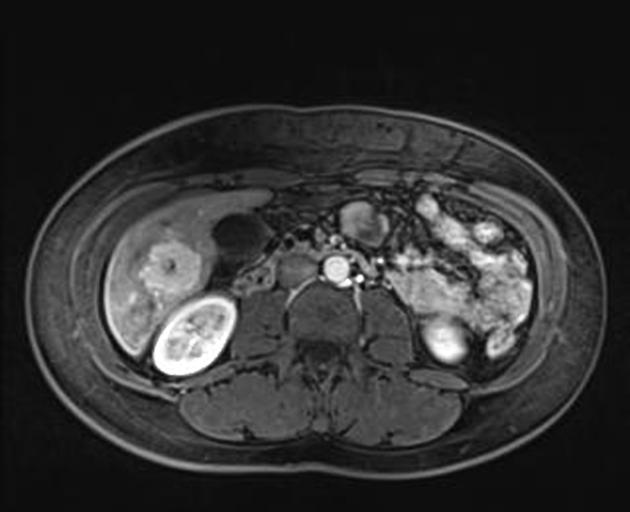
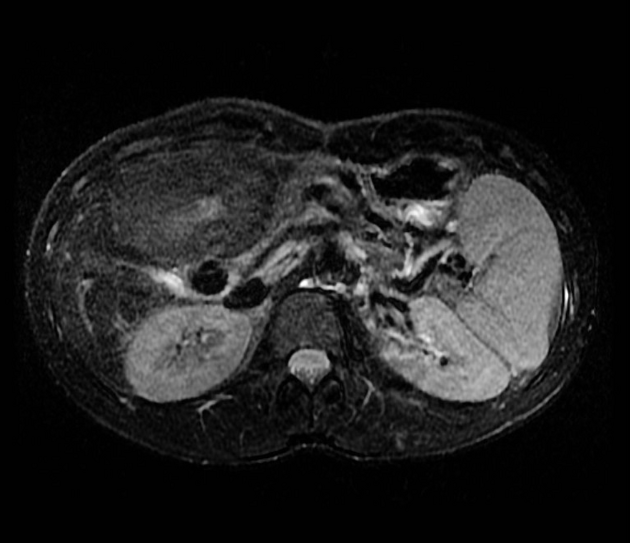
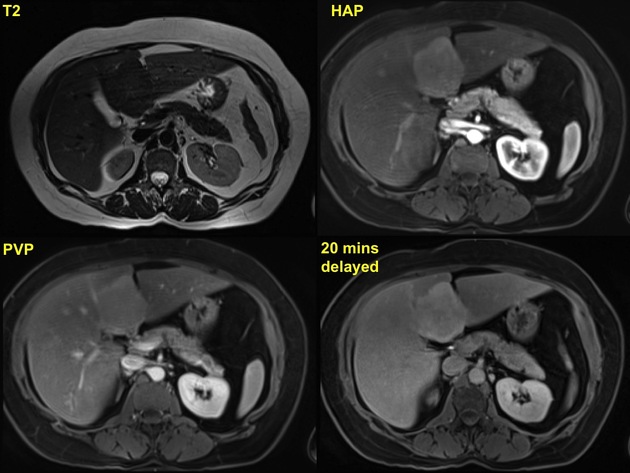
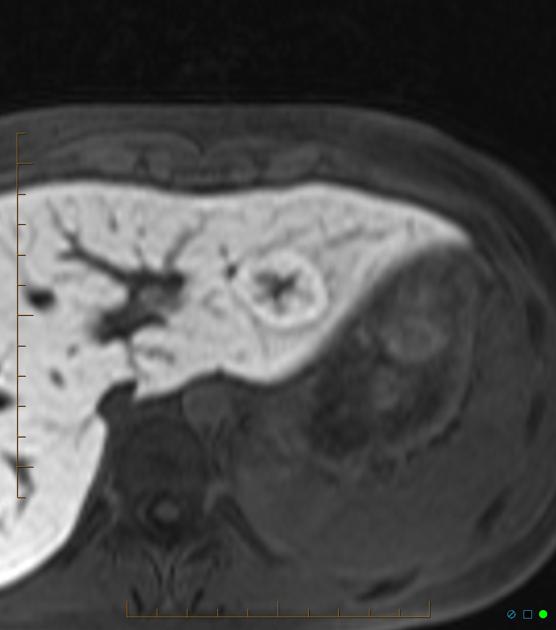
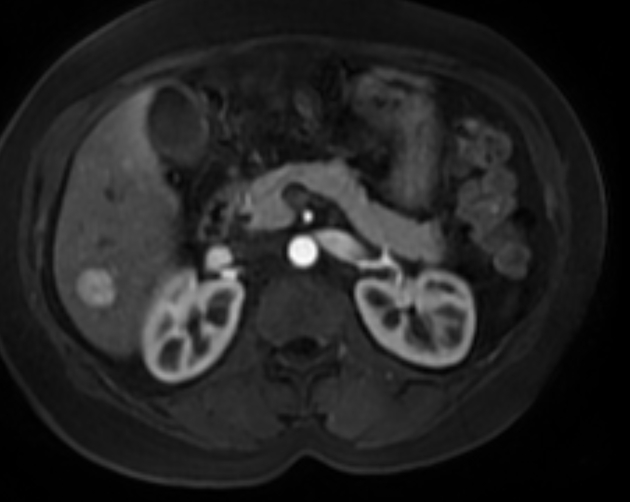
MRI
Liver MRI is both sensitive (70%) and specific (98%).
-
T1
iso to moderately hypointense
hypointense central scar
-
T2
iso to somewhat hyperintense
hyperintense central scar
-
T1 C+ (Gd)
central fibrotic scar retains contrast on delayed scans 13
slightly hyperintense or isointense to liver on portal venous phase 10-12,25
early intense arterial phase enhancement, similar to CT
-
T1 C+ (Eovist/Primovist)
early arterial enhancement
enhancement persists into delayed phases 11 to a greater degree than the background liver due to the presence of normal hepatocytes and abnormal bile ductules
fades toward background liver intensity on the delayed hepatobiliary phase, with a small amount of enhancement remaining (cf. adenomas, which are classically hypointense relative to liver on hepatobiliary phase)
central fibrotic scar typically does not enhance on hepatobiliary phase
-
T2* C+ (SPIO)
hypointense mass as a result of susceptibility signal loss due to uptake by Kupffer cells (cf. adenomas, which show a lower signal loss because of uptake by fewer Kupffer cells) 24
Nuclear medicine
Two radiopharmaceuticals can be used to image focal nodular hyperplasia: Tc-99m sulfur colloid and Tc-99m HIDA.
Sulfur colloid is taken up by the reticuloendothelial system, specifically the Kupffer cells which line the hepatic sinusoids 18. Because focal nodular hyperplasia is essentially focally malformed hepatic tissue, these lesions contain functioning Kupffer cells and take up technetium-99m sulfur colloid on nuclear imaging.
Classically, uptake pattern of Tc-99m sulfur colloid can be used to distinguish focal nodular hyperplasia from other liver lesions which do not contain normal liver cellularity, such as hepatic adenomas, hepatocellular carcinoma, and hepatic metastases. Focal nodular hyperplasia is associated with normal or increased radiotracer uptake, whereas the others are associated with focal decreased uptake 4. Intense focal uptake is thought to be quite specific for focal nodular hyperplasia 19.
That being said, up to 30% of focal nodular hyperplasia present with photopenia 19. Hepatic adenomas may rarely contain Kupffer cells and may be associated with normal uptake 19.
HIDA radiopharmaceuticals are taken up and excreted by hepatocytes in a similar way to bilirubin and bile. Since focal nodular hyperplasia contains all hepatic cell types (including hepatocytes and bile canaliculi) HIDA can be used to image focal nodular hyperplasia. Limited evidence suggests that HIDA scans might be more accurate than the more traditionally used sulfur colloid scan.
The usual HIDA scan findings consistent with focal nodular hyperplasia are increased blood flow, prompt hepatic uptake and delayed tracer clearance from the lesion. This pattern is reportedly seen in more than 90% of patients 23.
Treatment and prognosis
Focal nodular hyperplasia is benign, with no malignant potential and a minuscule risk of complication (rupture, hemorrhage) and thus are usually treated conservatively 1.
History and etymology
The term focal nodular hyperplasia was used initially by the American pathologist Hugh A Edmondson, in 1958 13.
Differential diagnosis
General imaging differential considerations include:
hepatic adenoma: usually more heterogeneous CT portal and delayed phases contrast washout; no gadoxetate retention on delayed phase MR and associated with fat, calcification or hemorrhage
hepatocellular carcinoma (HCC): usually in cirrhosis; vascular invasion
-
fibrolamellar (FL) hepatocellular carcinoma
both focal nodular hyperplasia and fibrolamellar hepatocellular carcinoma commonly have a hypointense "central scar" representing fibrosis, so this feature is less useful for differentiation
fibrolamellar hepatocellular carcinoma tends to appear more distinct from adjacent liver parenchyma on pre-contrast T1 / T2-weighted imaging
often larger (>12 cm)
calcification (uncommon in focal nodular hyperplasia), corresponding to necrosis and foreign body type reaction histopathologically 20
70% present with metastases, or evidence of biliary, vascular, and nodal invasion
decreased activity on Tc-99m / sulfur colloid scan
hypervascular hepatic metastases: usually multiple; CT portal and delayed phases hypodense (washout); older patients with known primary tumor
hepatic hemangioma: peripheral and centripetal enhancement; blood vessels isodense; no central scar; only small ones with rapid enhancement simulate focal nodular hyperplasia
intrahepatic cholangiocarcinoma: hypoenhancing in earlier arterial/venous phases with delayed enhancement, dominant large central scar 21
Practical points
in the setting of cirrhotic liver, be wary of diagnosing a hypervascular lesion as a focal nodular hyperplasia unless you have definitely excluded hepatocellular carcinoma
focal nodular hyperplasia typically has no capsule; if a hypervascular liver mass has a capsule, put hepatocellular carcinoma above focal nodular hyperplasia on the differential diagnosis
there is likely overlap in appearance between focal nodular hyperplasia and inflammatory hepatic adenoma when using gadoxetate sodium (Eovist/Primovist); if the patient has risk factors (e.g. metabolic syndrome), consider both in the differential diagnosis 15



















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.