Gallbladder polyps are commonly occurring elevated lesions on the mucosal surface of the gallbladder. The vast majority are benign. They are best characterized on ultrasound as a non-shadowing endophytic growth into the gallbladder lumen.
On this page:
Epidemiology
Gallbladder polyps are relatively frequent, seen in ~5% (range 0.3-12.3%) of the population 1,7,12,14,23. The majority are cholesterol polyps.
Cholesterol polyps are most frequently identified in patients between 40-50 years of age and are more common in women (F:M = 2.9:1) 3.
Associations
Patients with Peutz-Jeghers syndrome and familial adenomatous polyposis have an increased prevalence of pyloric gland adenomas within the gallbladder ref.
Clinical presentation
Gallbladder polyps are typically incidental findings in ~10% of upper abdominal ultrasound examinations. Unless large, polyps are usually asymptomatic 1,3.
Pathology
A wide variety of entities appear as polyps and histology is variable:
-
benign polyps (a.k.a. pseudopolyps): >70% all polyps 23
cholesterol polyps: >50% of all polyps 3,7,14
inflammatory polyps: ~10% 14
focal adenomyomatosis 13,23
other rare entities (see benign tumors and tumor-like lesions of the gallbladder)
-
non-invasive neoplastic polyps
pyloric gland adenoma of the gallbladder: present in <0.5% of cholecystectomy specimens for cholelithiasis or chronic cholecystitis, occasionally associated with familial adenomatous polyposis or Peutz-Jeghers syndrome 22
-
malignant polyps: most measure >20 mm
adenocarcinoma: ~90% of malignant polyps
-
and other rare entities including
lymphoma 23
squamous cell carcinoma
angiosarcoma
Radiographic features
In most instances, predicting histology based purely on imaging is not possible, with the possible exception of cholesterol polyps in some instances (see below), and thus features that are predictive of benign vs malignant disease should be noted (see benign vs malignant features of gallbladder polyps) 1,6,7.
Neoplastic polyps are larger, mean size of 18-21 mm compared to non-neoplastic polyps, mean size of 4-7.5 mm 18.
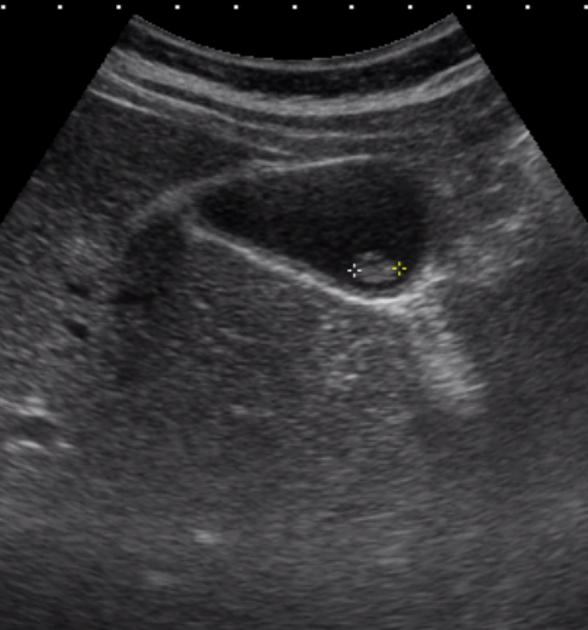
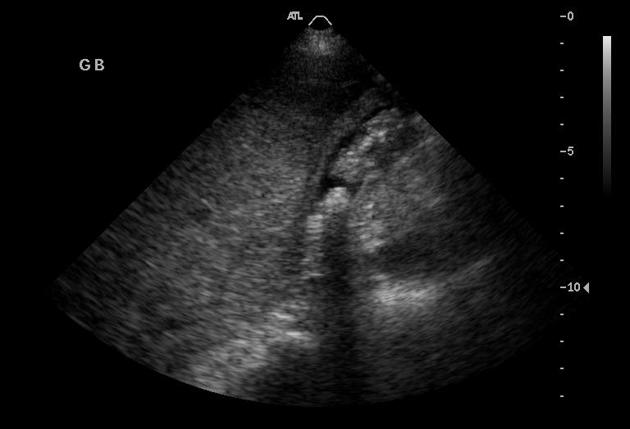
Ultrasound
Ultrasound is the best initial imaging choice and is often able to separate cholesterol polyps from those requiring treatment. General features of gallbladder polyps are a non-shadowing polypoid ingrowth into the gallbladder lumen, which is usually immobile unless there is a relatively long pedunculated component.
General features of polyps include 8:
-
small size
cholesterol polyps are the most frequent, over 90% are <10 mm, and the vast majority are <5 mm; they often have a single supplying vessel
benign neoplasms or malignant lesions tend to be larger
-
echogenicity varies with the size
small polyps are echogenic but non-shadowing
larger cholesterol polyps tend to be hypoechoic
-
morphology
small polyps may be adherent to the wall and smooth
larger lesions tend to be pedunculated and granular in outline
comet-tail artifact indicates a cholesterol polyp or focal adenomyomatosis 13
Rarely, endoscopic ultrasound may be useful to further assess gallbladder polyps as it may generate higher resolution images 7,8.
High-resolution ultrasound
Some publications have suggested a useful role in high-resolution ultrasound (HRUS) for categorization of gallbladder polyps with features favoring neoplastic polyps from benign comprising of 16:
size >1 cm
lobulated surface contour
presence of branching vessels seen on color Doppler
hypoechoic internal echo of the polyp
hypoechoic foci within the polyp
Contrast-enhanced ultrasound demonstrates vascular characteristics.
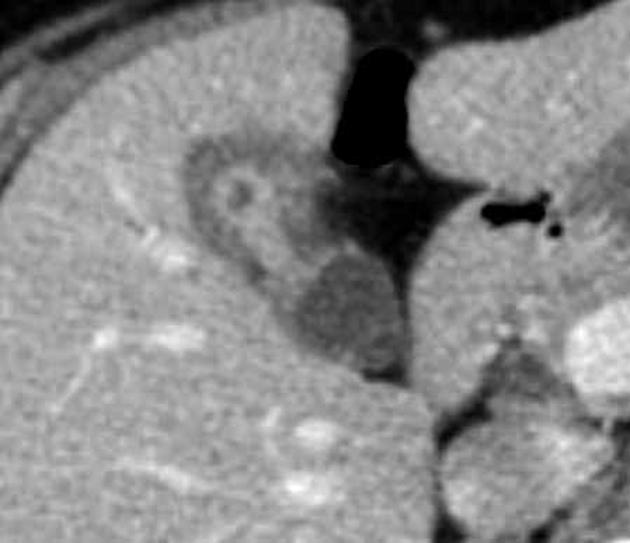
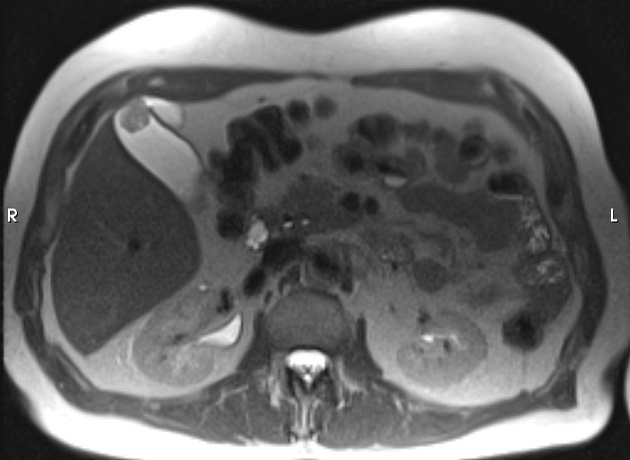
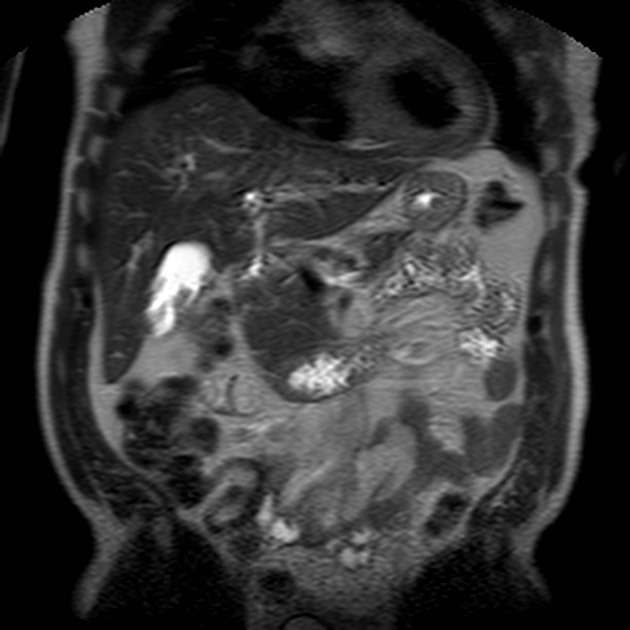
CT
CT is often unable to detect small gallbladder polyps. Larger polyps will appear as soft tissue attenuation projections into the lumen of the gallbladder and will demonstrate enhancement similar to that of the rest of the gallbladder. More intense enhancement should be viewed with suspicion, as it is associated with increased vascularity in malignancy.
Treatment and prognosis
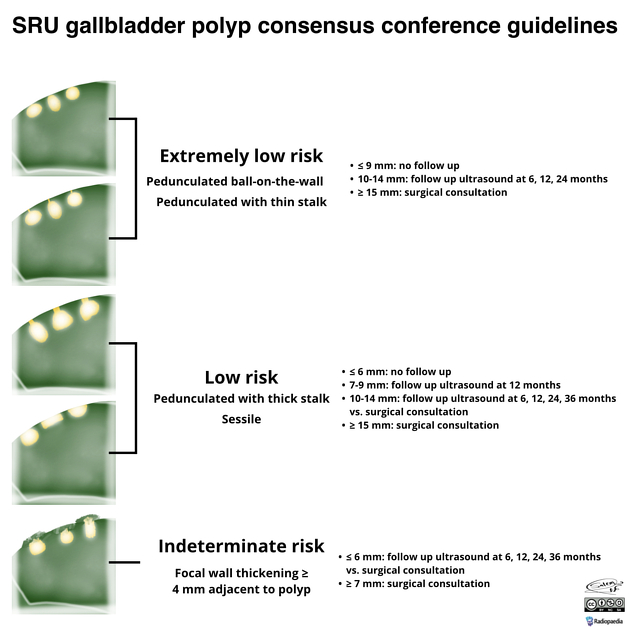
Society of Radiologists in Ultrasound guidelines (2021)
The Society of Radiologists in Ultrasound (SRU) found no link between gallbladder carcinoma and polyps 17. Most gallbladder cancers arise from flat dysplastic epithelium that thickens as the cancer progresses. They recognize three categories of polyps: non-neoplastic, benign neoplastic, and malignant. The follow-up period is shortened to 3 years. Concerning growth is increased to >4 mm per annum. Slow growth of benign polyps up to 2 mm per annum is common, and conversely, many small polyps disappear. Most malignant polyps are >20 mm.
According to the 2021 guidelines:
-
extremely low risk polyps (pedunculated ball-on-the-wall, or thin stalk):
≤9 mm: no follow-up
10-14 mm: follow-up ultrasound at 6, 12, and 24 months
≥15 mm: surgical consultation
-
low risk polyps (pedunculated with thick stalk, or sessile):
≤6 mm: no follow-up
7-9 mm: follow-up ultrasound at 12 months
10-14 mm: follow-up ultrasound at 6, 12, 24, and 36 months or surgical consultation
≥15 mm: surgical consultation
-
indeterminate risk polyps (focal wall thickening ≥4 mm adjacent to polyp):
≤6 mm: follow-up ultrasound at 6, 12, 24, and 36 months or surgical consultation
≥7 mm: surgical consultation
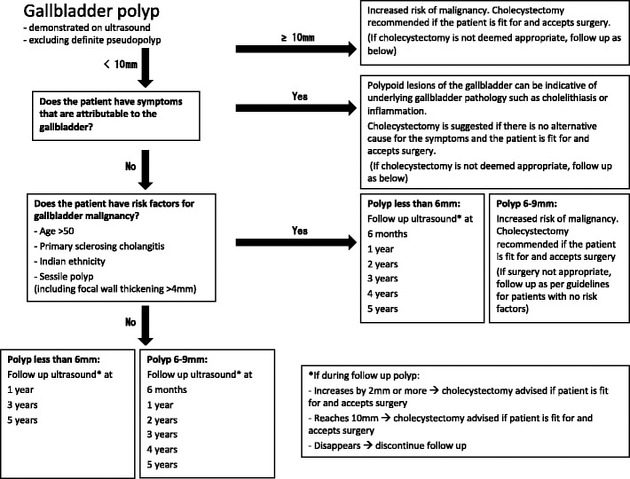
European guidelines (2022)
In 2022, the joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), European Association for Endoscopic Surgery and other Interventional Techniques (EAES), International Society of Digestive Surgery - European Federation (EFISDS) and European Society of Gastrointestinal Endoscopy (ESGE) 13 were updated 24:
-
polyp ≥10 mm
cholecystectomy recommended if no alternative cause for the symptoms is demonstrated
-
polyp <10 mm
symptoms attributable to the gallbladder: cholecystectomy is recommended if no alternative cause for the symptoms is determined (polyp may be indicative of underlying occult calculus or inflammation)
-
no symptoms attributable to the gallbladder:
-
if the patient has one or more risk factors* for gallbladder malignancy:
-
polyp 6-9 mm
cholecystectomy recommended
-
polyp ≤5 mm
follow-up ultrasound at 6 months, 1 year and 2 years
-
-
no risk factors for gallbladder malignancy:
-
polyp 6-9 mm
follow-up ultrasound at 6 months, 1 year and 2 years
-
polyp ≤5 mm
follow-up not required
-
-
*Risk factors: >60 years, primary sclerosing cholangitis, Asian ethnicity, sessile polyp (including focal wall thickening >4 mm).
If a polyp grows ≥2 mm within 2 years, its size should be considered along with risk factors.
Statistically, gallbladder polyps are common and gallbladder cancer is rare, so very few polyps progress to gallbladder cancer. There is also controversy regarding the development of gallbladder cancer and some suggest that polyps may not progress to cancer 10.
American College of Radiology guidelines (2013)
According to the White Paper of the ACR Incidental Findings Committee II on Gallbladder and Biliary Findings (2013) 11:
≤6 mm: no further evaluation or follow-up necessary 6,10
7-9 mm: yearly follow-up with an ultrasound to ensure no interval growth 15
-
≥10 mm: surgical consultation for cholecystectomy
if no cholecystectomy, annual follow-up is justified 11
Lower thresholds for follow-up or intervention may be warranted if the patient population is known to have a higher risk of gallbladder carcinoma (e.g. higher incidences in Pakistan, Ecuador, and females in India).
Differential diagnosis
The differential for a gallbladder polyp is limited, and includes 6:
-
usually mobile, but can be adherent
usually cast an acoustic shadow
gallbladder metastases (especially in patients with a history of melanoma)
gallbladder fold, if inadequately distended









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.