Hepatocellular carcinoma (HCC), also called hepatoma, is the most common primary malignancy of the liver. It is strongly associated with cirrhosis, from both alcohol and viral etiologies. Hepatocellular carcinomas constitute approximately 5% of all cancers partly due to the high endemic rates of hepatitis B infection 1.
On this page:
Epidemiology
Hepatocellular carcinoma is the fifth most common cancer in the world and is the third most common cause of cancer-related death (after lung and stomach cancer). The incidence of hepatocellular carcinoma is rising, largely attributable to a rise in hepatitis C infection 2.
The highest prevalence occurs in Asia, in regions where chronic hepatitis B infection is endemic, and this accounts for >80% of hepatocellular carcinoma cases worldwide. In Western countries, the rate of hepatitis B infection is lower and alcohol accounts for the majority of cases.
Hepatocellular carcinoma is typically diagnosed in late middle-aged or elderly adults (average 65 years) and is more common in males (75% of cases) 7. In regions where chronic hepatitis B infection is endemic, young adults aged 20 to 40 (who had contracted the virus via maternal-fetal transmission) have the highest risk of developing hepatocellular carcinoma 1.
Hepatocellular carcinoma also occurs in the pediatric population and is the second most common pediatric primary liver tumor after hepatoblastoma.
Fibrolamellar hepatocellular carcinoma is a distinct variant of hepatocellular carcinoma not associated with cirrhosis and has different demographics and risk factors.
Risk factors
Risk factors include 1:
hepatitis B (HBV) infection: 10% 5-year cumulative risk 3
hepatitis C (HCV) infection: 30% 5-year cumulative risk
alcohol use: 8% 5-year cumulative risk
biliary cholangitis: 5% 5-year cumulative risk
food toxins, e.g. aflatoxins
congenital biliary atresia
-
inborn errors of metabolism
hemochromatosis: ~20% 5-year cumulative risk
tyrosinemia type I 4
obesity and diabetes mellitus 6
Diagnosis
The diagnosis of hepatocellular carcinoma is usually established by imaging and/or pathology 28-31.
With appropriate imaging, such as multiphasic CT or dynamic MRI, the diagnosis can be made in high-risk patients, e.g. with hepatitis B and/or cirrhosis, using characteristic contrast enhancement patterns, without the need for histological confirmation 28-31.
In patients without cirrhosis and hepatitis B infection, the diagnosis is made by histology 28-32.
Diagnostic criteria
Essential diagnostic criteria according to the WHO classification of digestive system tumors (5th edition) 32:
histological proof of hepatocellular differentiation
histological proof of malignancy
absence of heterotypic, non-hepatocellular differentiation
In critical cases, histological evidence should be potentially supported by immunohistochemistry 6.
Molecular analysis is not required but can help with the identification of subtypes and the diagnosis of difficult cases 6.
Diagnostic clues
Diagnosis on imaging is mainly supported by the LI-RADS algorithm and is based on imaging features including arterial hyperenhancement, portal venous or delayed washout, capsular enhancement, tumor size and threshold growth 30.
Clinical presentation
The presentation is variable and, in affluent nations, is often found in the setting of screening programs for patients with known risk factors 8. Otherwise, the presentation may include:
constitutional symptoms
portal hypertension from the invasion of the portal vein
hepatomegaly/mass
hemorrhage from tumor
Pathology
The origin of hepatocellular carcinomas is believed to be related to repeated cycles of necrosis and regeneration, irrespective of the cause. Additionally, the genomes of HBV and HCV contain genetic material that may predispose cells to accumulate mutations or disrupt growth control, thus allowing for a second mechanism by which infection with these agents predisposes to hepatocellular carcinoma 1.
Macroscopic appearance
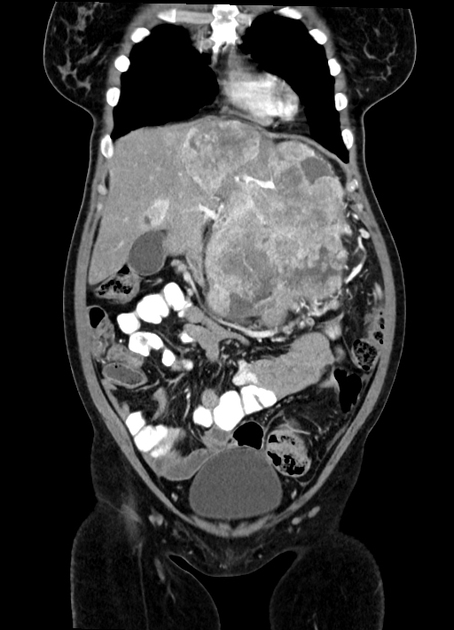
On gross pathology, hepatocellular carcinomas typically appear as pale masses within the liver and may be unifocal, multifocal or diffusely infiltrative at the time of presentation.
The macroscopic growth of hepatocellular carcinoma is usually categorized into three subtypes: nodular, massive and infiltrative. Each has different radiological features, which are detailed below 9. The infiltrative subtype is characterized by the growth of multiple tiny nodules throughout the entire liver or an entire liver segment.
Microscopic appearance
Microscopically they range from well-differentiated to undifferentiated.
Markers
alpha-fetoprotein (AFP) levels are elevated in 50-75% of cases 2
Radiographic features
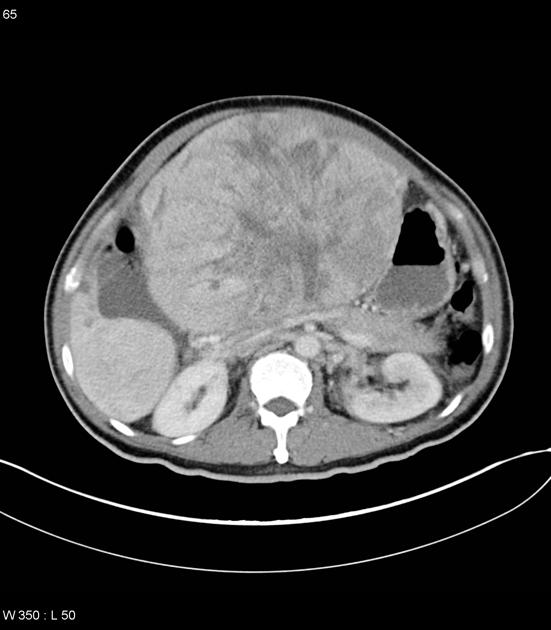
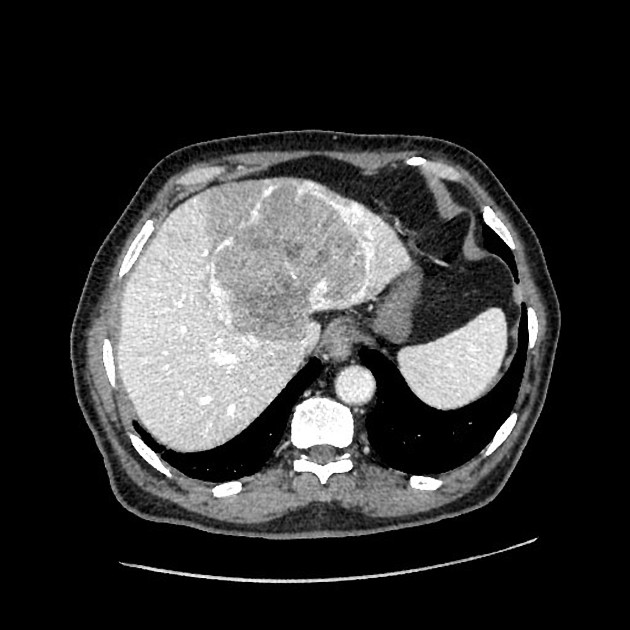
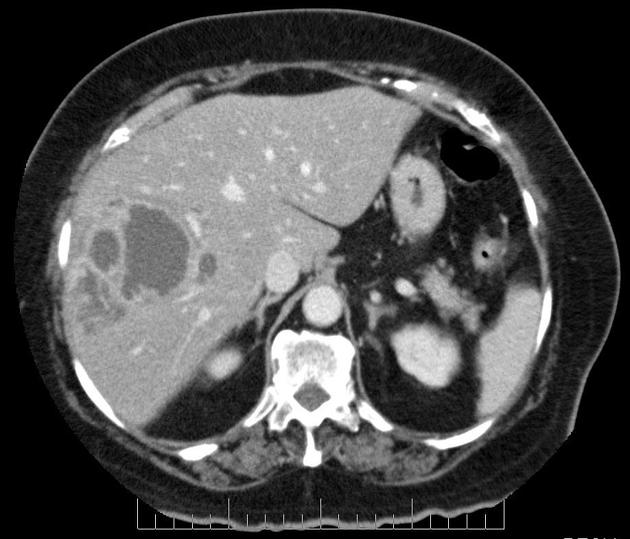
Hepatocellular carcinomas can have a variety of appearances:
-
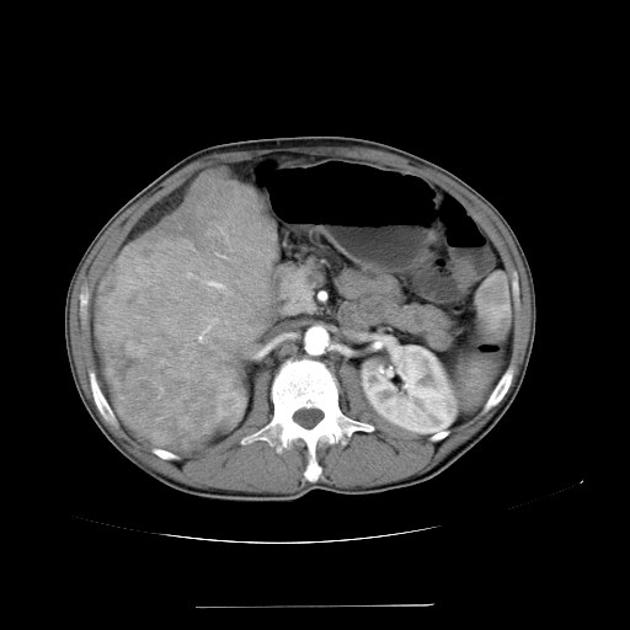
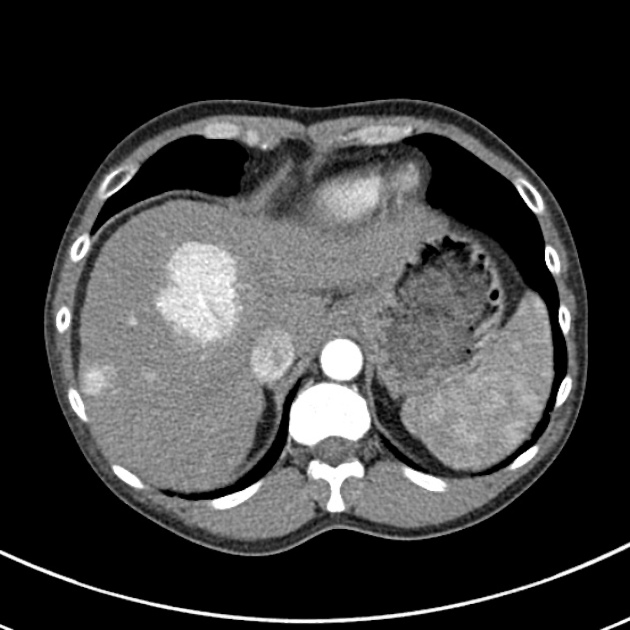
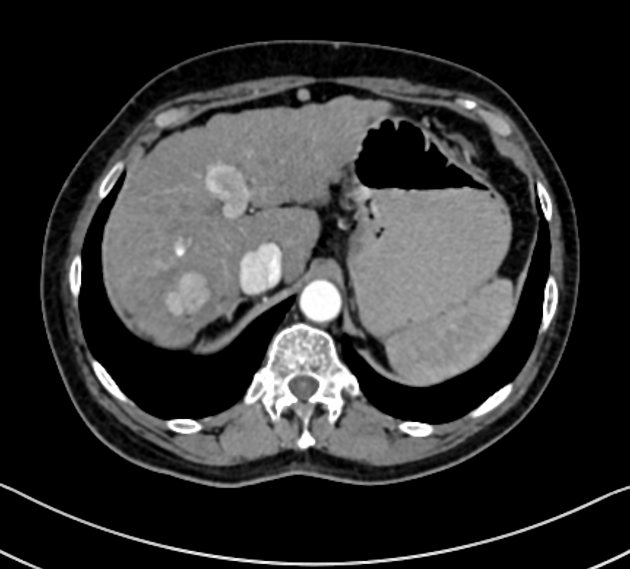
massive (focal)
large mass
may have necrosis, fat and /or calcification
-
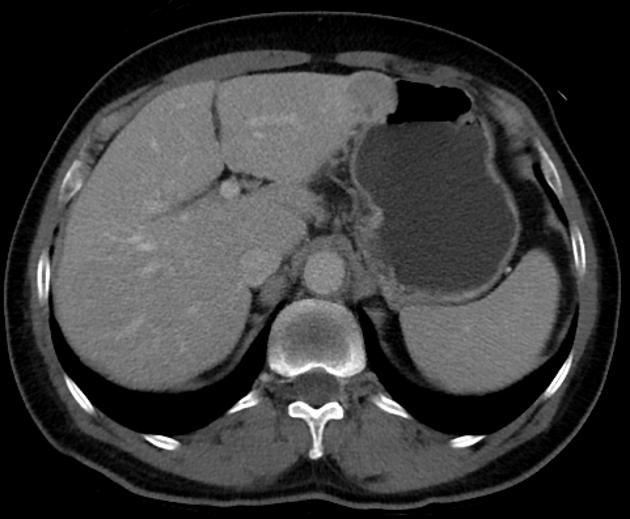
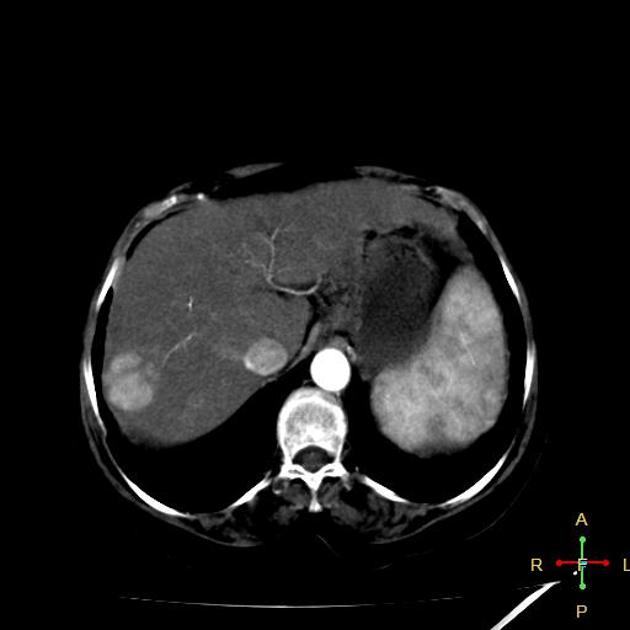
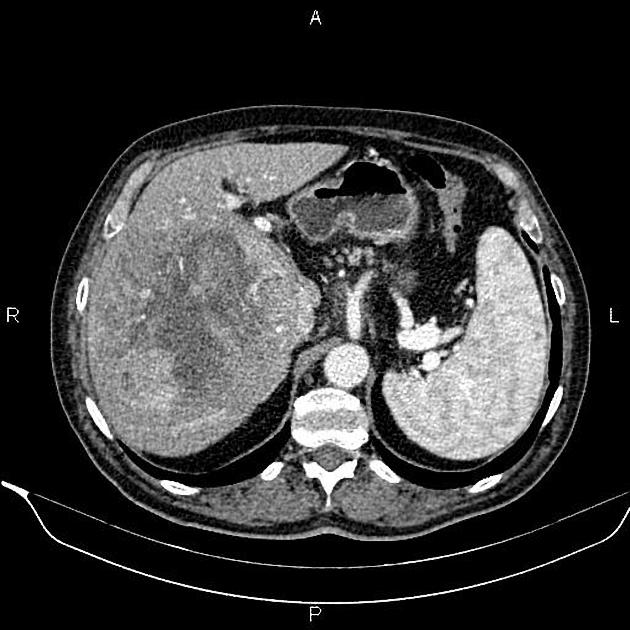
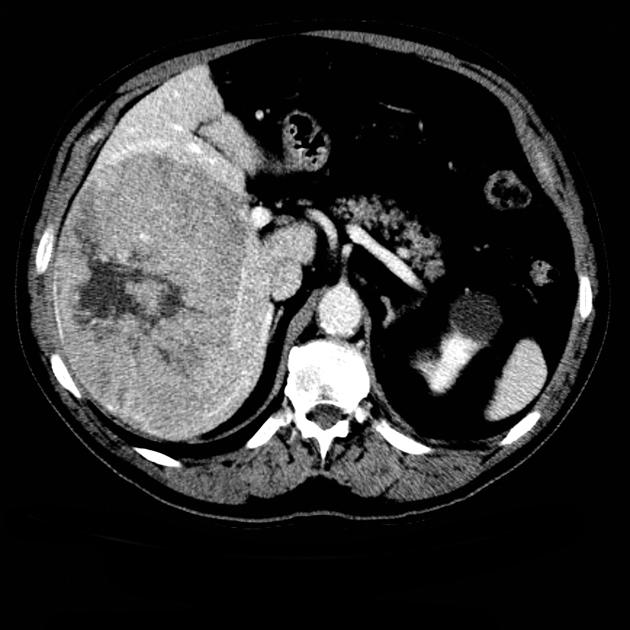
nodular (multifocal)
multiple masses of variable attenuation
may also have central necrosis
-
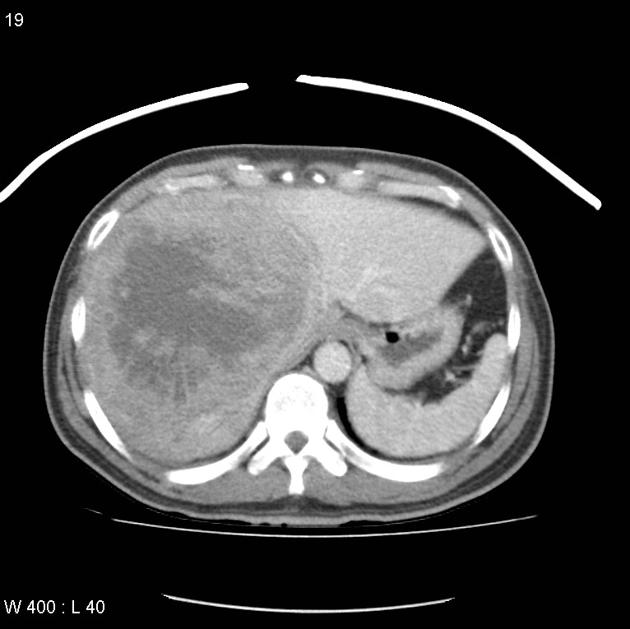
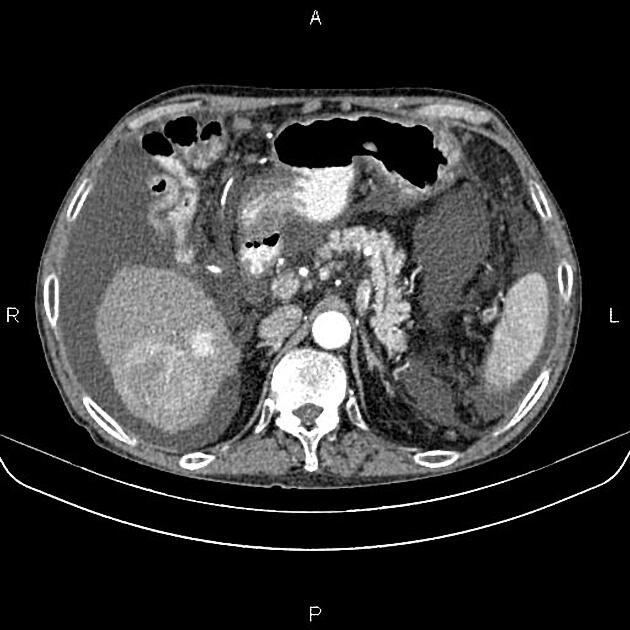
infiltrative (diffuse) 10
may difficult to distinguish from associated cirrhosis: also called cirrhotomimetic-type hepatocellular carcinoma or cirrhosis-like hepatocellular carcinoma
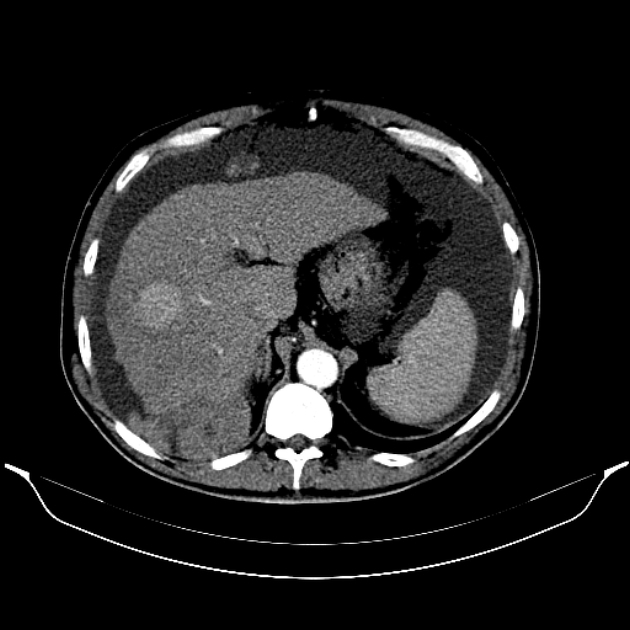
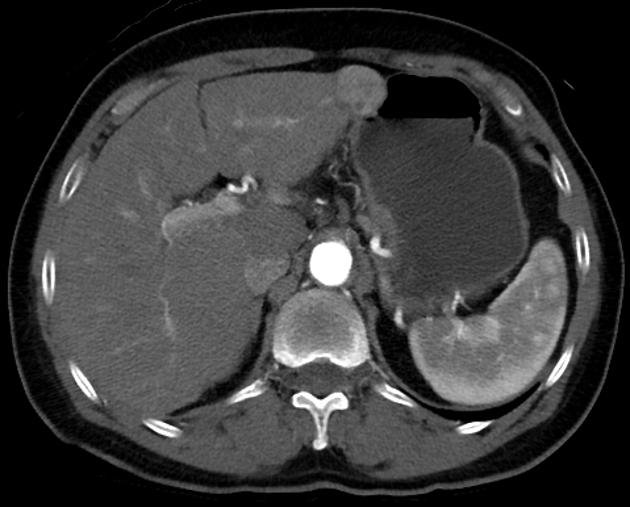
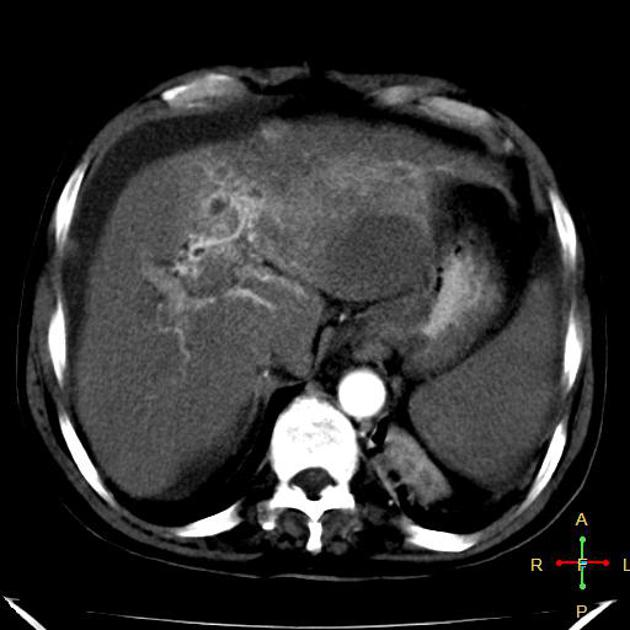
Hepatocellular carcinoma receives most of its blood supply from branches of the hepatic artery, accounting for its characteristic enhancement pattern: early arterial enhancement with early "washout." Hence, small foci of hepatocellular carcinoma may be seen within a regenerative liver nodule as foci of arterial enhancement (nodule-in-nodule appearance) 11.
Hepatocellular carcinoma uncommonly demonstrates a central scar similar to focal nodular hyperplasia but may be differentiated by the absence of delayed contrast enhancement of the scar (as seen in focal nodular hyperplasia).
Rim enhancement on delayed post-contrast images causing a capsule appearance is considered relatively specific for hepatocellular carcinoma (see case 4).
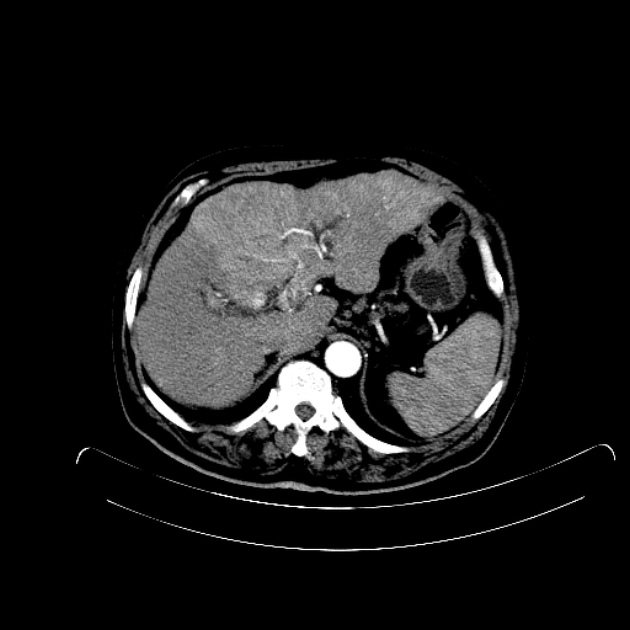
Additionally, these tumors have the propensity to invade vascular structures, most commonly the portal vein, but also the hepatic veins, IVC, and right atrium. One should remember that a large number of patients will have concomitant cirrhosis, and thus also be at risk for bland portal vein thrombosis from synthetic dysfunction of clotting factors.
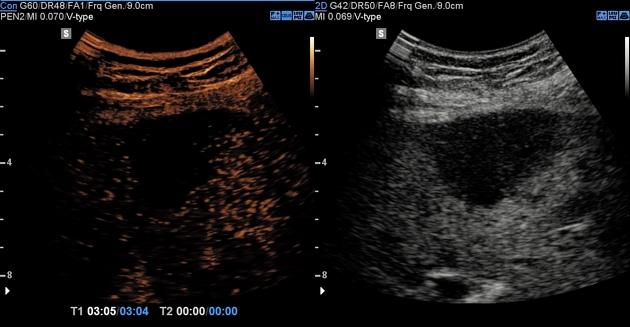
Ultrasound
Variable appearance, depending on the individual lesion, size, and echogenicity of the background liver. Typically:
small focal hepatocellular carcinoma appears hypoechoic compared with normal liver
larger lesions are heterogeneous due to fibrosis, fatty change, necrosis and calcification 12
a peripheral halo of hypoechogenicity may be seen with focal fatty sparing (see the discussion below on the CT session)
diffuse hepatocellular carcinoma may be difficult to identify or distinguish from background cirrhosis
-
contrast-enhanced ultrasound 13
-
arterial phase
arterial enhancement from neovascularity
-
portal venous phase
decreased echogenicity relative to background liver ("washout")
tumor thrombus may be visible
variants have been described with arterial phase hypovascularity with no enhancement or arterial enhancement with no "washout"
-
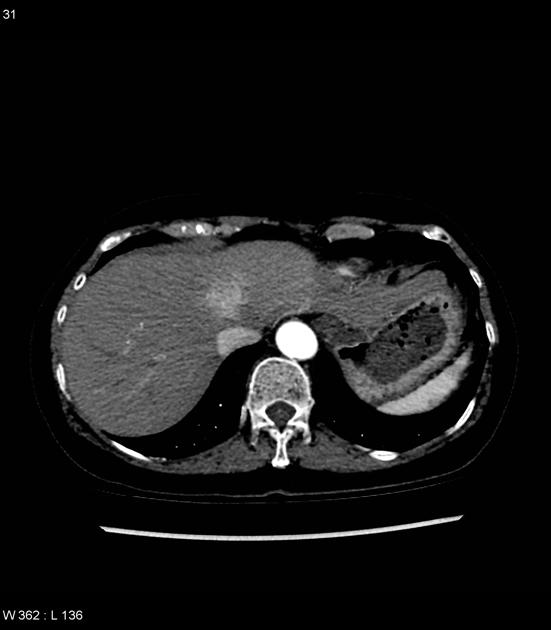
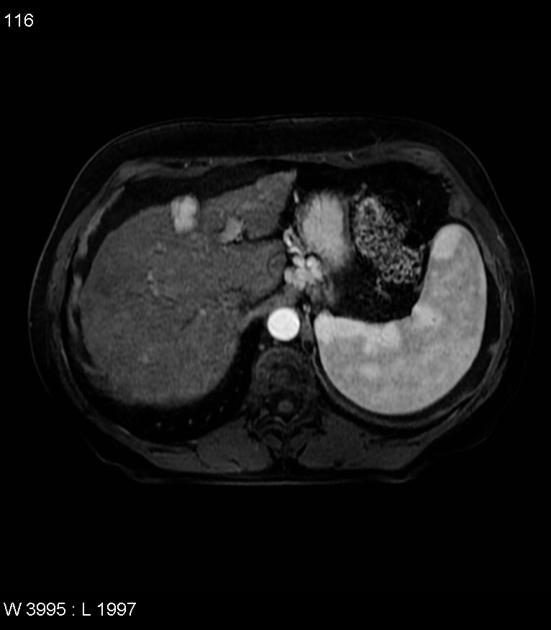
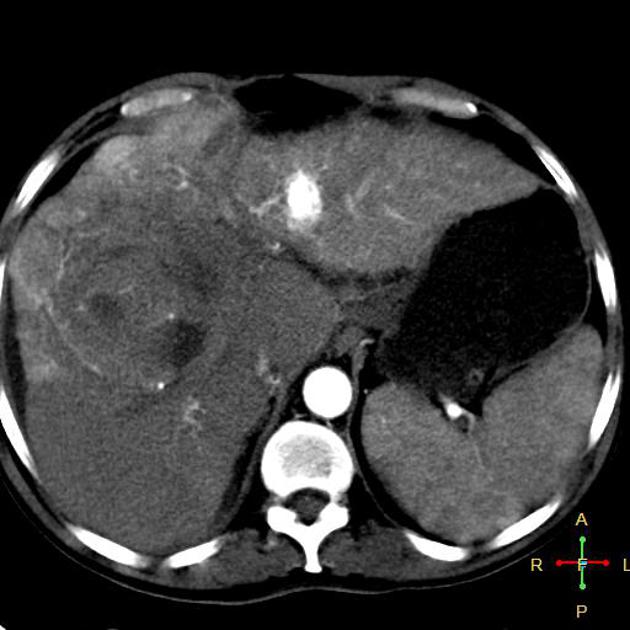
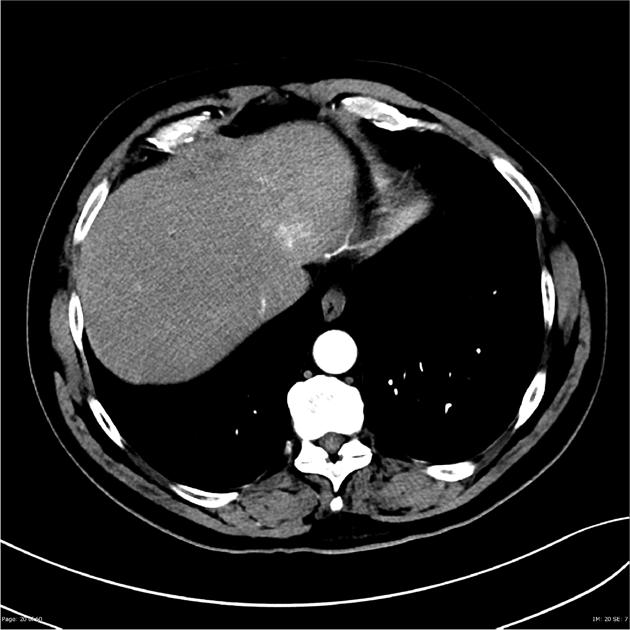
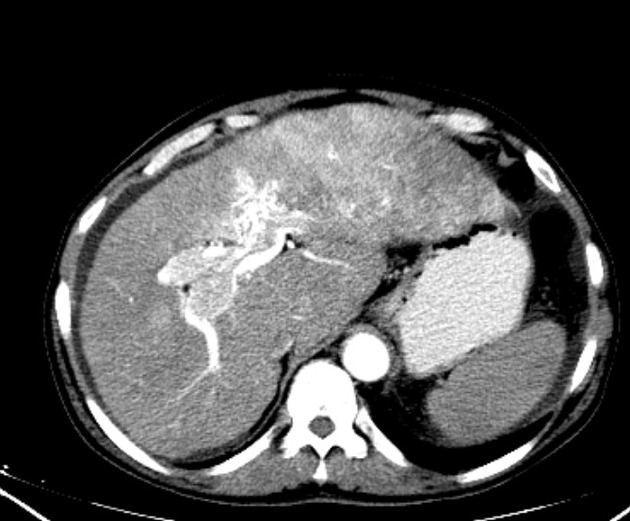
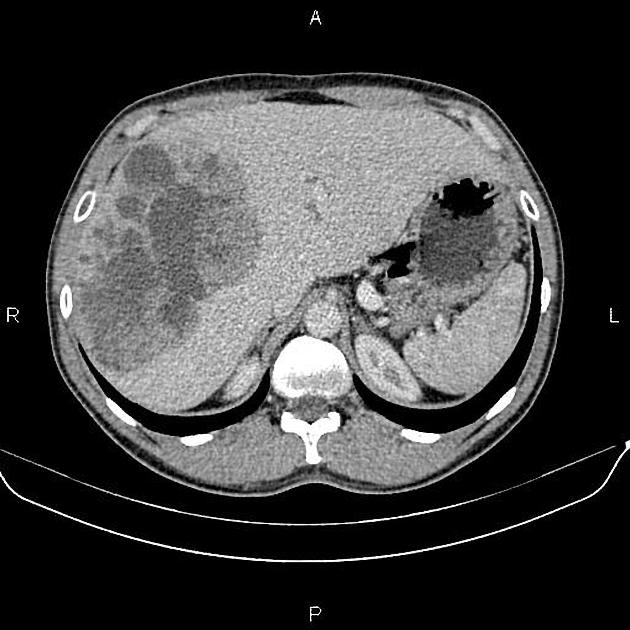
CT
Several patterns can be seen, depending on the subtype of hepatocellular carcinoma. Enhancement pattern is the key to the correct assessment of hepatocellular carcinomas.
Usually, the mass enhances vividly during late arterial (~35 seconds) and then washes out rapidly, becoming indistinct or hypoattenuating in the portal venous phase, compared to the rest of the liver.
Additionally, they may be associated with a wedge-shaped perfusion abnormality due to arterioportal shunts (APS), and this, in turn, can result in a focal fatty change in the normal liver or focal fatty sparing in the diffusely fatty liver 14. A halo of focal fatty sparing may also be seen around a hepatocellular carcinoma in an otherwise fatty liver 15.
Portal vein tumor thrombus can be distinguished from bland thrombus by demonstrating enhancement.
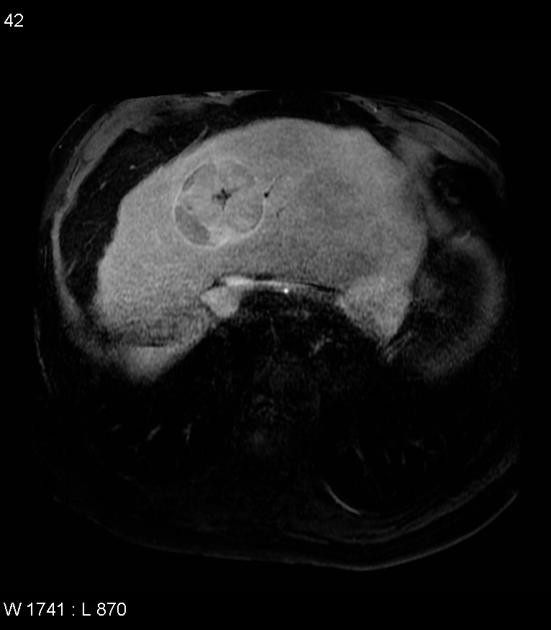
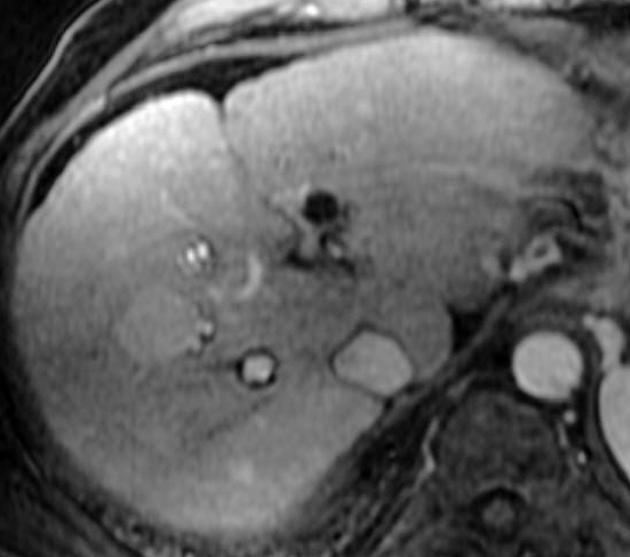
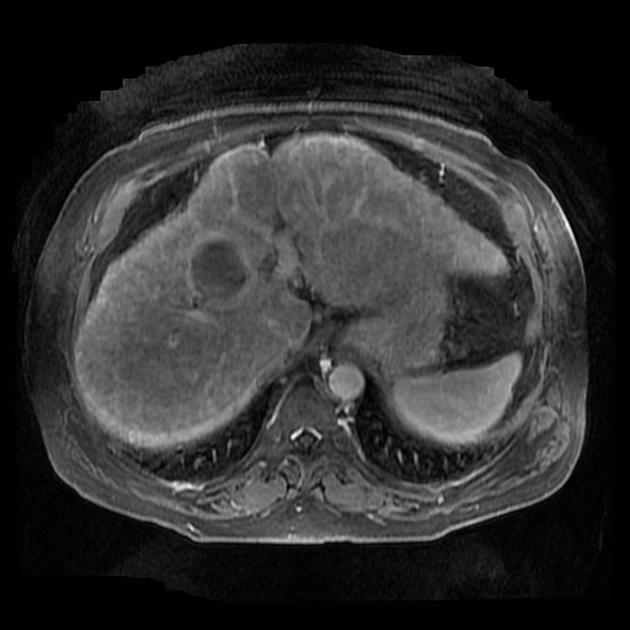
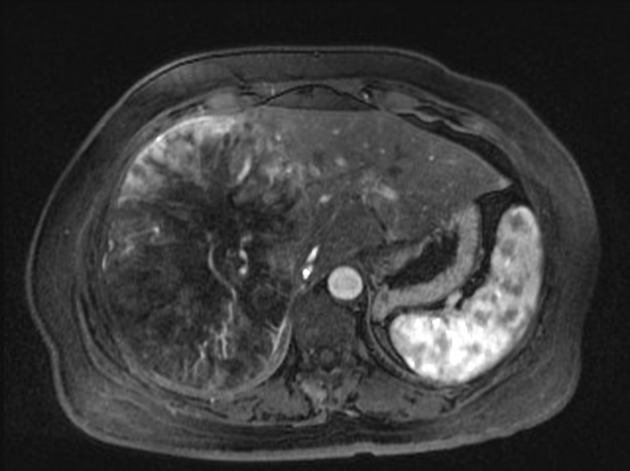
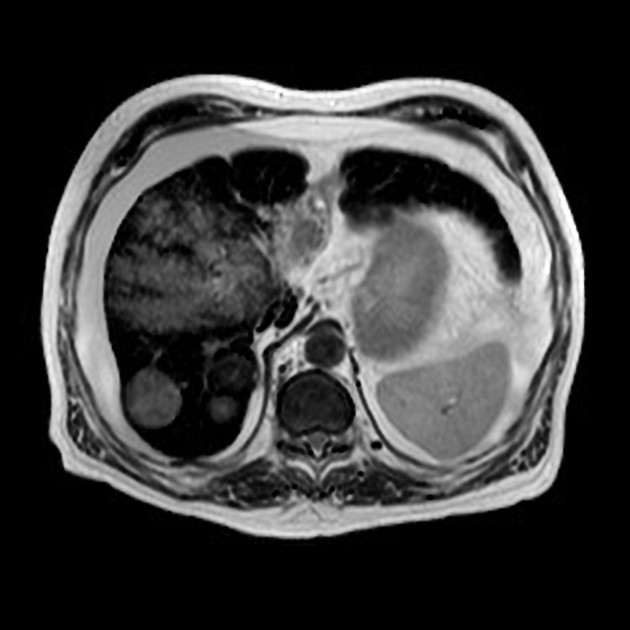
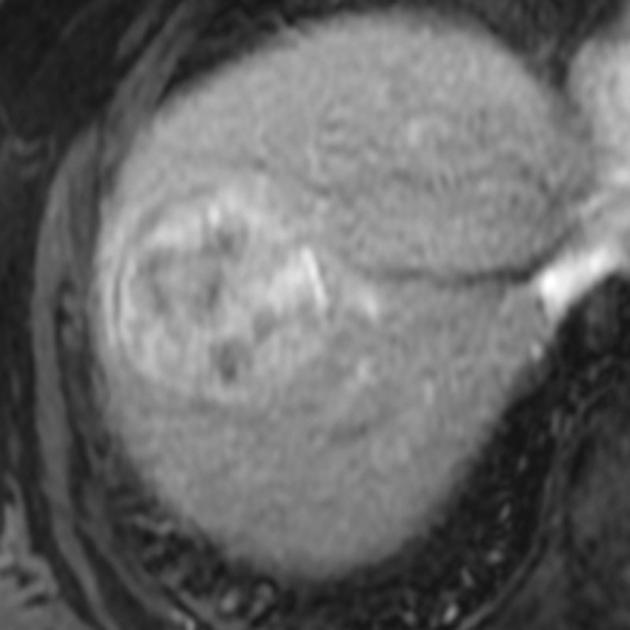
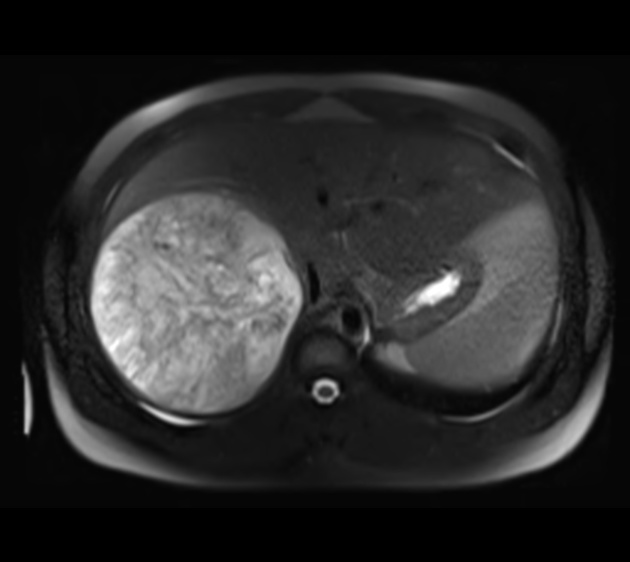
MRI
In the setting of cirrhosis, small hepatocellular carcinomas need to be distinguished from regenerative and dysplastic nodules 16.
In general, the MRI signal is:
-
T1
variable
iso- or hypointense to surrounding liver 17
-
hyperintensity may be due to
intratumoral fat 3
decreased intensity in the surrounding liver
-
T1 C+ (Gd)
enhancement is usually arterial ("hypervascularity")
-
rapid "washout", becoming hypointense to the remainder of the liver (96% specific) 3
this is because the supply to hepatocellular carcinoma is predominantly from the hepatic artery rather than the portal vein
rim enhancement may persist ("capsule")
an imaging classification system (LI-RADS) has been developed to stratify lesions
-
T1 C+ (hepatobiliary agents: Eovist, Primovist)
-
similar to assessment with extracellular gadolinium, but evaluation of the hepatobiliary phase requires care
most commonly arterial phase hyperenhancement (APHE) with portal venous washout 33
washout on the transitional phase (3 minutes delayed) is less reliable (see: Eovist and LI-RADS)
well-differentiated HCC can have absent APHE and appear hypointense on hepatobiliary phase 33
10-15% will retain contrast on the hepatobiliary phase, typically in well-differentiated HCCs with functional hepatocytes 33,34
-
T2: variable, typically moderately hyperintense
C+ post-SPIO (iron oxide): increases sensitivity in diagnosing small hepatocellular carcinomas
DWI: intratumoral high signal; increases sensitivity and specificity 33
Angiography (DSA)
hyper vascular tumor
threads and streaks pattern: sign of tumor thrombus in the portal vein
PET Imaging
18F-FDG PET is a valuable tool in assessing extrahepatic disease, but its assessment in identifying HCC from normal liver tissue is less promising. Well-differentiated hepatocellular carcinoma is the most common histopathological pattern and thus resembles normal hepatocytes and shows similar metabolism. Therefore, 18F-FDG PET is less sensitive for these lesions. Poorly differentiated HCCs or HCCs with high proliferation index show increased metabolic activity and thus are easily detectable 35. 68Ga labeled PSMA has also shown promising results, as PSMA is expressed in vascular channels of HCC 36.
Treatment and prognosis
Treatment options are improving; minimally invasive surgical techniques reduce the complication rate and the combination of newer radiofrequency ablation techniques with transarterial chemoembolisation TACE) can be comparable or safer 37. TACE enhances thermocoagulation by reducing intra-tumoral blood circulation and cooling. It can also treat micrometastases.
The typical TNM staging system seen in most other epithelial cancers is not as prognostically useful for the stratification of patients with hepatic cancers. Early recurrence within 2 years implies an aggressive initial tumor type, whereas late recurrence after 2 years suggests de novo tumor and a better prognosis 37.
There are several substitute staging systems used in guiding therapy for hepatocellular carcinoma (see hepatocellular carcinoma staging) 18. The LI-RADS imaging classification system is also used to stratify lesions in an at-risk liver.
If the lesion is small then resection is possible (partial hepatectomy) and may result in remission. The remarkable ability of the liver to regenerate means that up to two-thirds of the liver can be resected 19.
Liver transplantation is also a curative option. To be suitable for liver transplantation it is agreed that certain criteria should be met (see Milan criteria).
If neither of these options are possible, then a variety of options exist including chemotherapy, transarterial chemoembolisation (TACE), transarterial radioembolization (TARE) / selective internal radiation therapy (SIRT), thermal ablation (RFA, cryoablation, or microwave ablation), and chemical ablation 20-22.
If a tumor is resectable, then 5-year survival is ~45% (range 37-56%) 23.
Metastasis occurs in the final stages of the disease (IVa) and carries a poor prognosis 24,25. The most frequently involved sites are the lung, adrenal glands, lymph nodes, and bone.
Differential diagnosis
General imaging differential considerations include:
-
hypervascular hepatic metastases
metastases to a cirrhotic liver are rare, often due to primary endocrine tumor
less venous invasion
-
focal nodular hyperplasia (FNH)
no vascular invasion or neovascularization
may have a non-enhancing surrounding "halo" or central scar
early arterial Eovist enhancement persists into delayed phases
Tc-99m sulphur colloid 80% positive
-
different demographics and risk factors
-
intrahepatic cholangiocarcinoma
peripheral location
biliary obstruction
delayed enhancement
hepatic tuberculoma 27
























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.