Acute pancreatitis (plural: pancreatitides) is an acute inflammation of the pancreas and potentially life-threatening.
On this page:
Terminology
Two subtypes of acute pancreatitis are described in the Revised Atlanta Classification 1:
-
interstitial edematous pancreatitis
the vast majority (90-95%)
most often referred to simply as "acute pancreatitis" or "uncomplicated pancreatitis"
-
necrosis develops within the pancreas and/or peripancreatic tissue
Epidemiology
The demographics of patients affected by acute pancreatitis reflect the underlying cause, of which there are many (see Pathology below).
Diagnosis
The diagnosis of acute pancreatitis is usually based on clinical criteria or a combination of clinical and radiographic features 1.
Diagnostic criteria
Two of the following three criteria are required for the diagnosis 1:
acute onset of persistent, severe epigastric pain (i.e. pain consistent with acute pancreatitis)
characteristic imaging features on contrast-enhanced CT, MRI, or ultrasound
Clinical presentation
Classical clinical features include 3:
acute onset of severe central epigastric pain (over 30-60 min)
poorly localized tenderness and pain
exacerbated by supine positioning
radiates through to the back in 50% of patients
Elevation of serum amylase and lipase are 90-95% specific for the diagnosis 3.
A normal amylase level (normoamylasaemia) in acute pancreatitis is well-recognized, especially when it occurs on the ground of chronic pancreatitis. A normal lipase level has also been reported (<10 case reports) but is extremely rare 16.
(Rare) signs of hemorrhage on the physical exam include:
Cullen sign: periumbilical bruising
Grey-Turner sign: flank bruising
Pathology
There continues to be debate over the precipitating factor leading to acute pancreatitis, with duct occlusion being an important factor, but neither necessary nor sufficient.
Mechanism notwithstanding, activation of pancreatic enzymes within the pancreas rather than the bowel leads to inflammation of the pancreatic tissue, disruption of small pancreatic ducts, and leakage of pancreatic secretions. Because the pancreas lacks a capsule, the pancreatic juices have ready access to surrounding tissues. Pancreatic enzymes digest fascial layers, spreading the inflammatory process to multiple anatomic compartments.
Etiology
gallstone passage/impaction: most common cause of acute pancreatitis (up to 15% develop pancreatitis)
-
idiopathic: 20% (range 10%-30%) of cases of acute pancreatitis
evidence suggests that most cases are associated with congenital duct abnormalities
-
alcohol use: most common cause of chronic pancreatitis
-
non-linear dose-response relationship 10
1.2x risk with ~40 g/day alcohol consumption
4x risk with ~100 g/day alcohol consumption
-
-
metabolic disorders
-
hypertriglyceridemia-induced pancreatitis 13
1-4% of cases
most common cause in pregnancy
hypercalcemia
-
penetrating peptic ulcer
-
trauma: most common cause in children
blunt abdominal trauma
surgery
-
malignancy
hereditary pancreatitis (autosomal dominant) SPINK1 gene mutation 5
malnutrition
-
infection
viral: mumps, Coxsackievirus, hepatitis, infectious mononucleosis, HIV/AIDS
parasitic: ascariasis 5, clonorchiasis
-
structural: not a cause, but associated with increased incidence
-
xenobiotics 32
antimicrobials (e.g isoniazid, metronidazole, tetracycline)
antiseizure medications (e.g. carbamazepine, sodium valproate)
analgesics (acetaminophen, non-steroidal anti-inflammatory drugs)
antiretrovirals (didanosine, nelfinavir)
cardiovascular (statins, loop diuretics, ACE inhibitors)
endocrine (estrogens, corticosteroids, gliptans)
immunosuppressants (mesalamine, azathioprine)
-
envenomations
Tityus trinitatis 27
Buthus quinquestriatus 31
-
others
scorpion stings/spider bites
See: causes of pancreatitis (mnemonic)
Complications
-
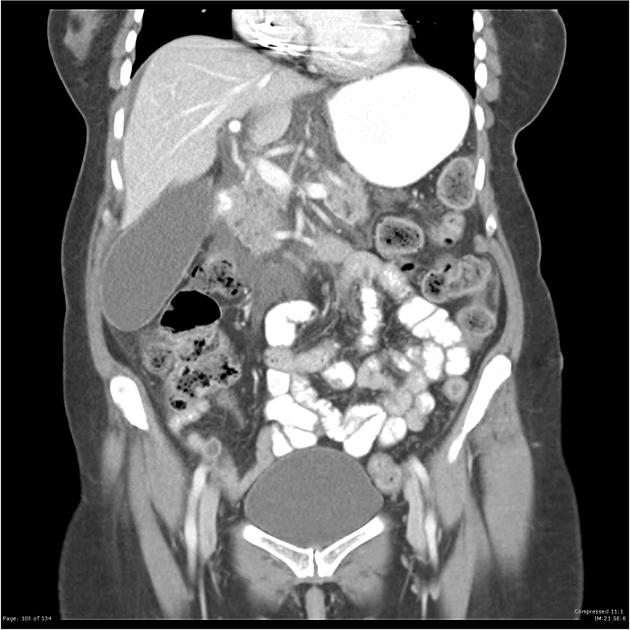
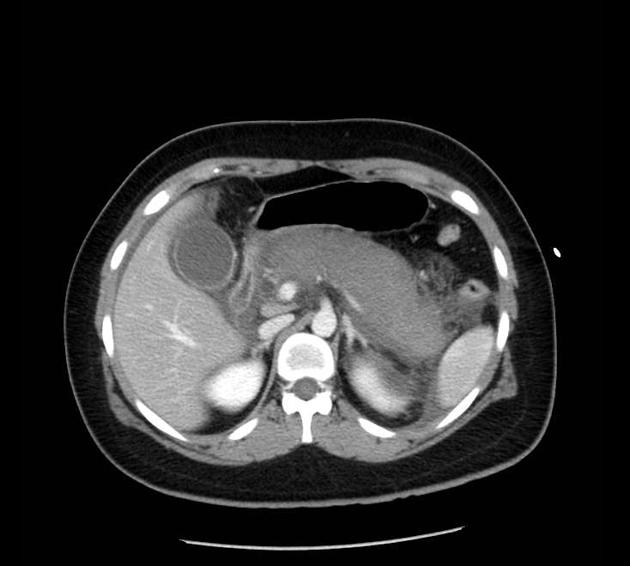
pancreatic fluid collections are defined by presence or absence of necrosis (as described by the Revised Atlanta Classification):
-
necrosis absent (i.e. interstitial edematous pancreatitis)
acute peripancreatic fluid collections (APFCs) (in the first 4 weeks)
pseudocysts: encapsulated fluid collections after 4 weeks
-
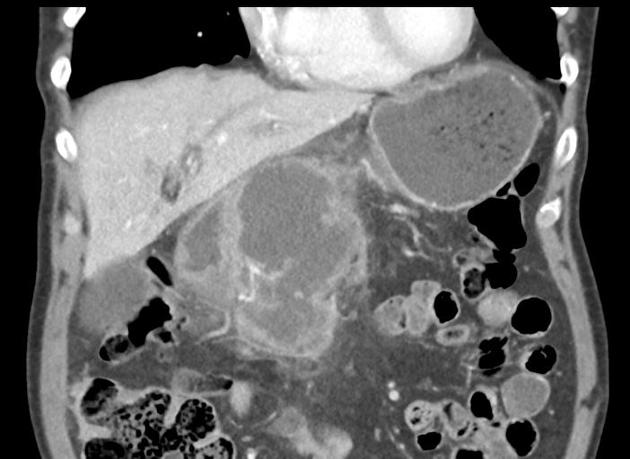
necrosis present (i.e. necrotizing pancreatitis)
acute necrotic collections (ANCs): develop in the first 4 weeks
walled-off necrosis (WON): encapsulated collections after 4 weeks
-
-
liquefactive necrosis of pancreatic parenchyma (e.g. necrotizing pancreatitis)
increased morbidity and mortality
may become secondarily infected (emphysematous pancreatitis)
-
vascular complications
hemorrhage: resulting from erosion of blood vessels and tissue necrosis
pseudoaneurysm: autodigestion of arterial walls by pancreatic enzymes results in pulsatile mass that is lined by fibrous tissue and maintains communication with parent artery
fistula formation with pancreatic ascites: leakage of pancreatic secretions into the peritoneal cavity
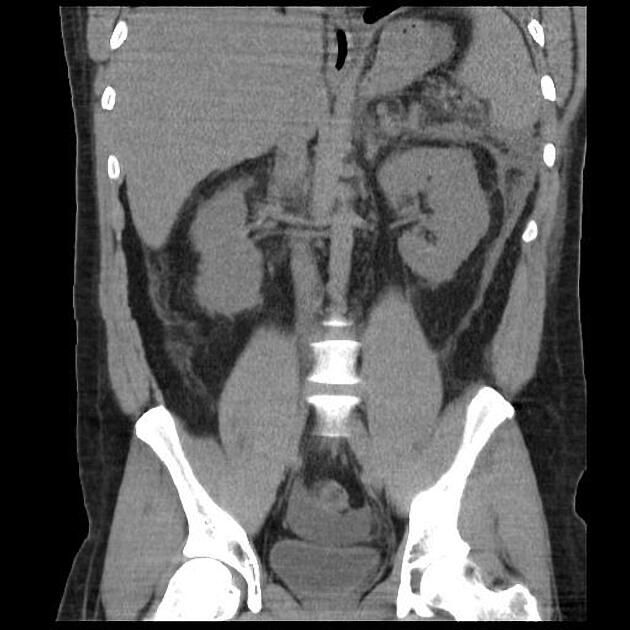
Radiographic features
The role of imaging is manifold:
to clarify the diagnosis when the clinical picture is confusing
to assess severity (e.g. Balthazar score) and thus to determine prognosis
to detect complications
to determine possible causes
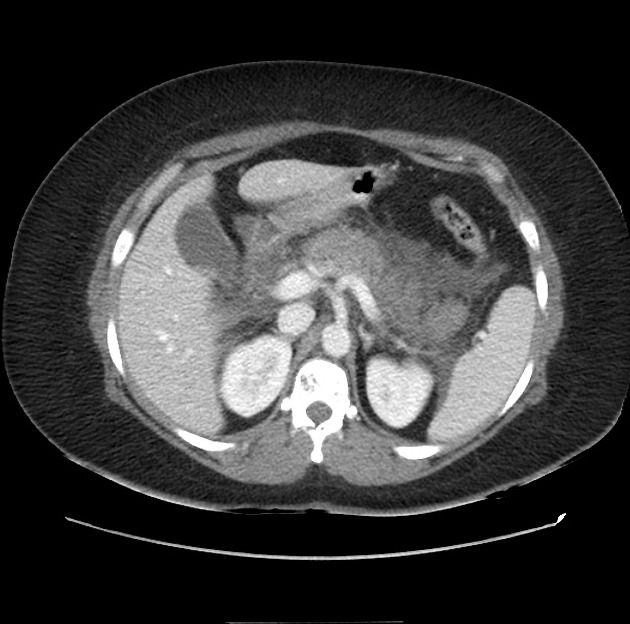
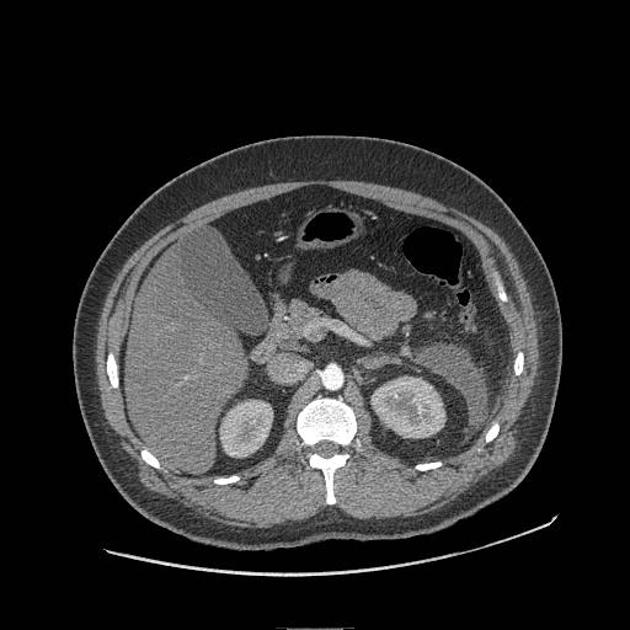
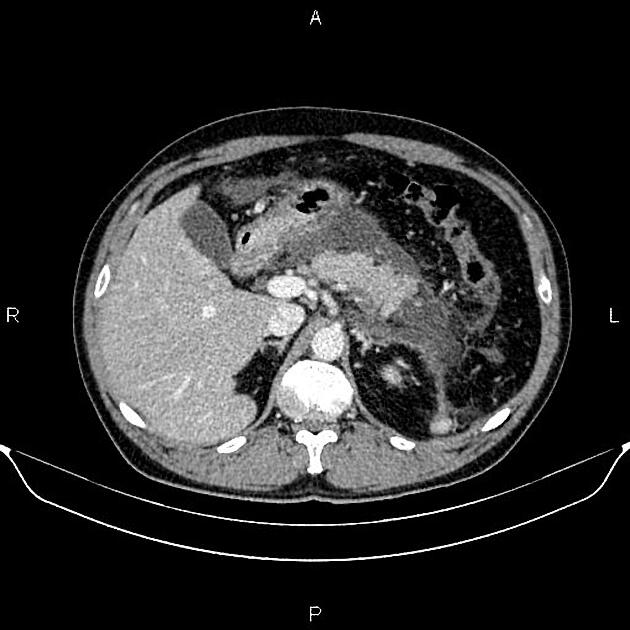
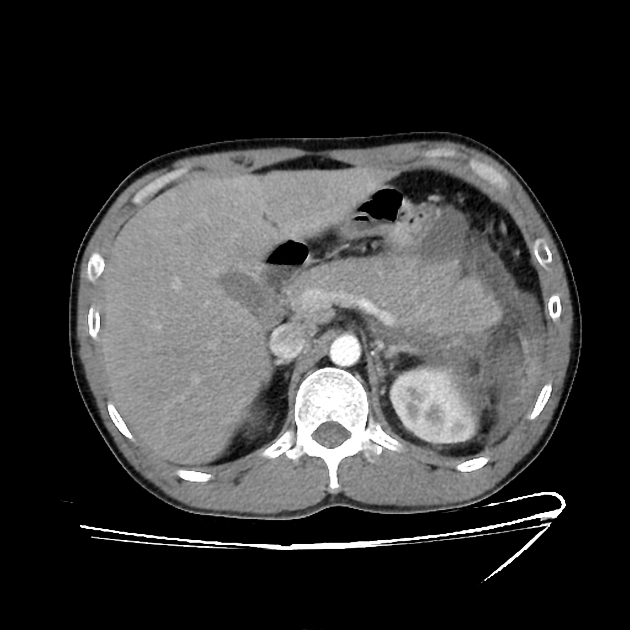
Imaging studies of acute pancreatitis may be normal in mild cases. Contrast-enhanced CT provides the most comprehensive initial assessment, typically with a dual-phase (arterial and portal venous) protocol. However, ultrasound is useful for the follow-up of specific abnormalities, such as fluid collections and pseudocysts.
Plain radiograph
Radiographs are insensitive for evidence of acute pancreatitis: many patients have normal exams. Moreover, none of the signs is specific enough to establish the diagnosis of pancreatitis.
Abdominal radiographs may demonstrate:
localized ileus of the small intestine (sentinel loop)
spasm of the descending colon (colon cut-off sign)
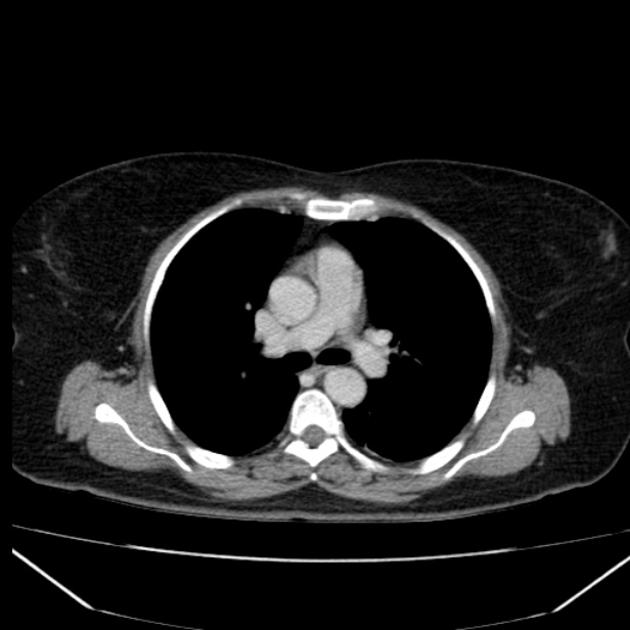
Chest radiographs may demonstrate:
pleural effusion, usually left-sided 25
basal atelectasis
pulmonary edema suggestive of acute respiratory distress syndrome
Ultrasound
The main role of ultrasound is:
to identify gallstones as a possible cause
diagnosis of vascular complications, e.g. thrombosis
identify areas of necrosis that appear as hypoechoic regions
assessment of clinically similar etiologies of an acute abdomen
In the event of a serendipitously patent acoustic window, typical ultrasonographic features congruent with acute pancreatitis include:
-
increased pancreatic volume with a marked decrease in echogenicity 19
volume increase quantified as a pancreatic body exceeding 2.4 cm in diameter, with marked anterior bowing and surface irregularity 17
decreased echogenicity secondary to fluid exudation, which may result in a marked heterogeneity of the parenchyma 18
displacement of the adjacent transverse colon and/or stomach secondary to pancreatic volume expansion 20
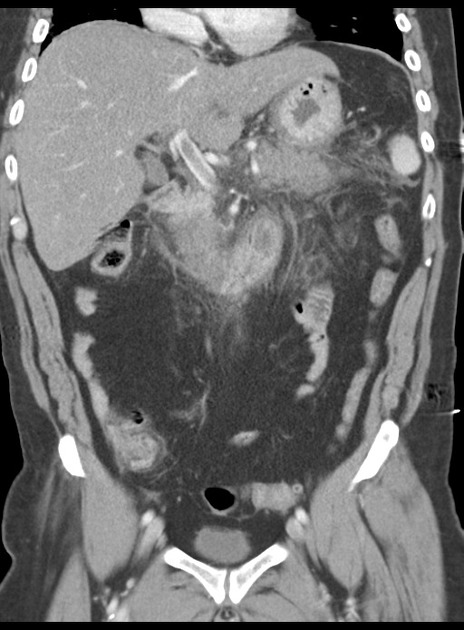
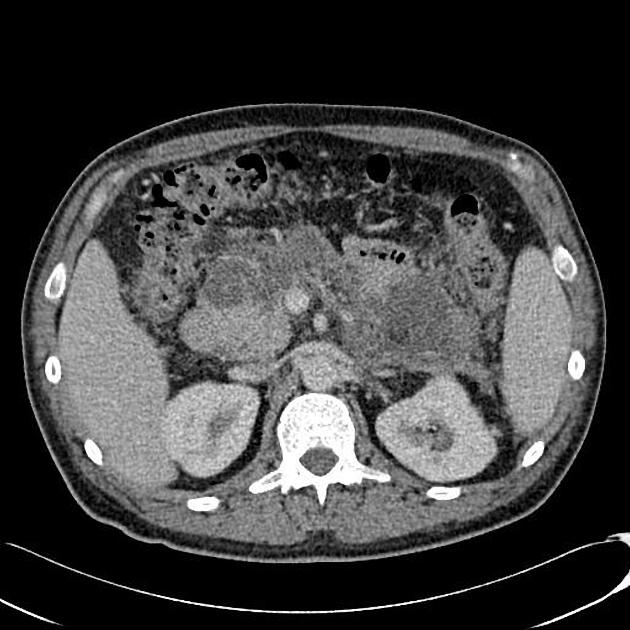
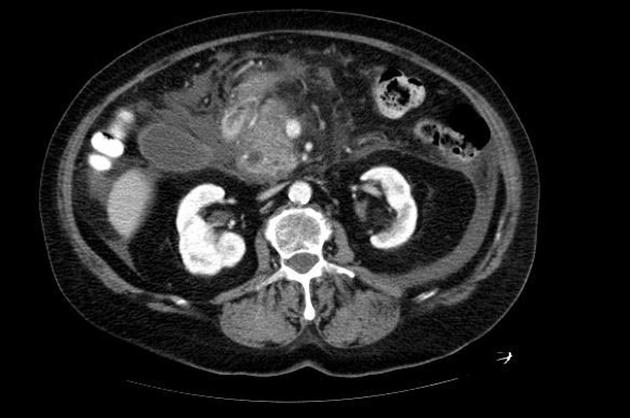
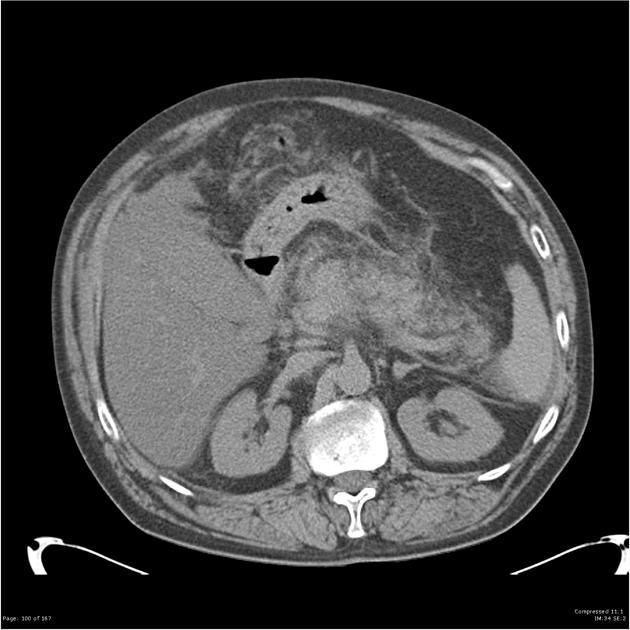
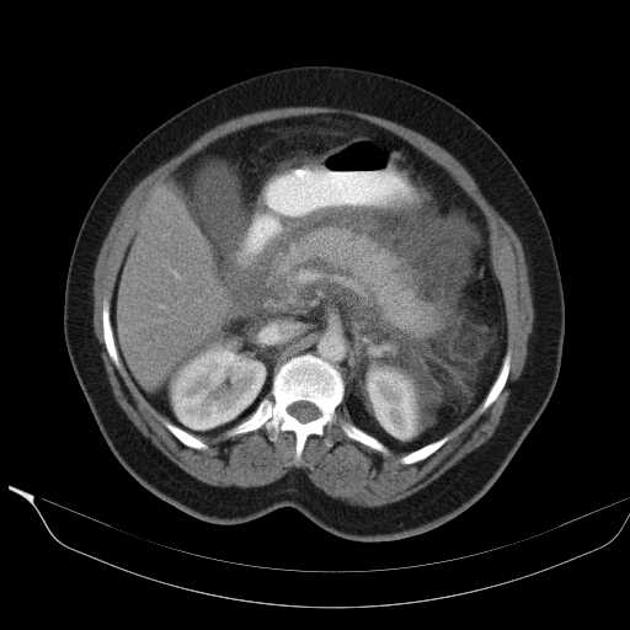
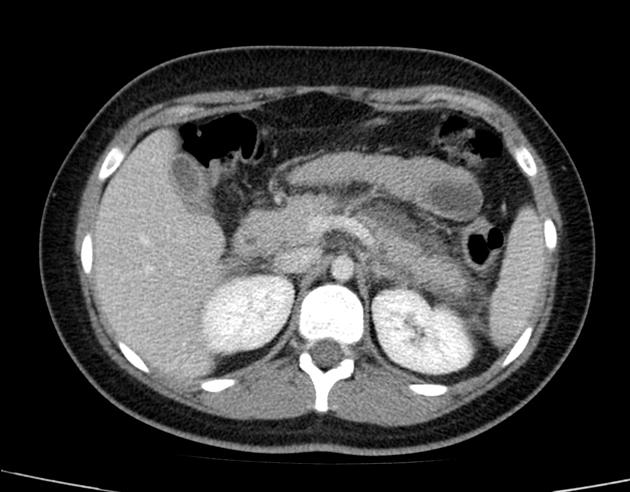
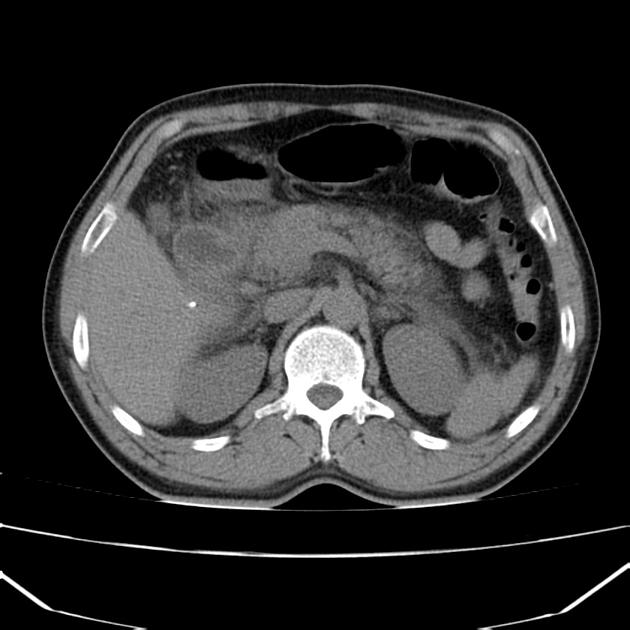
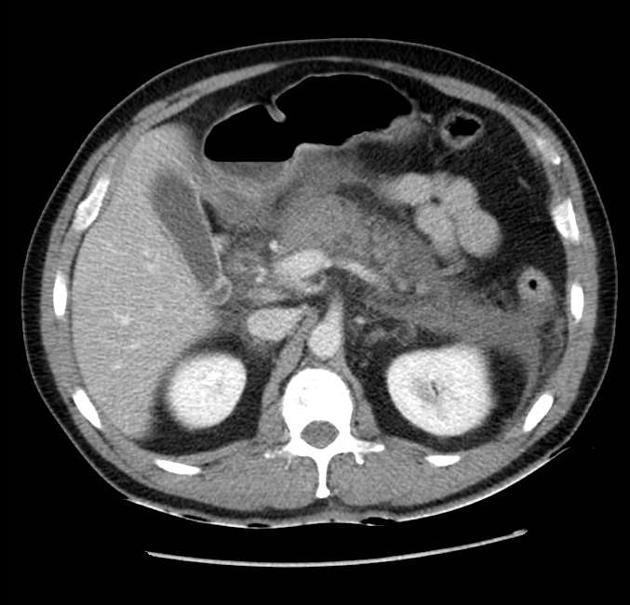
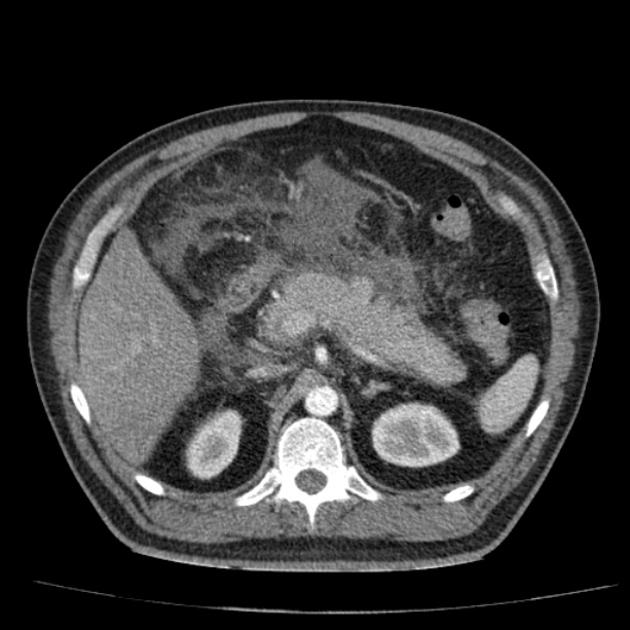
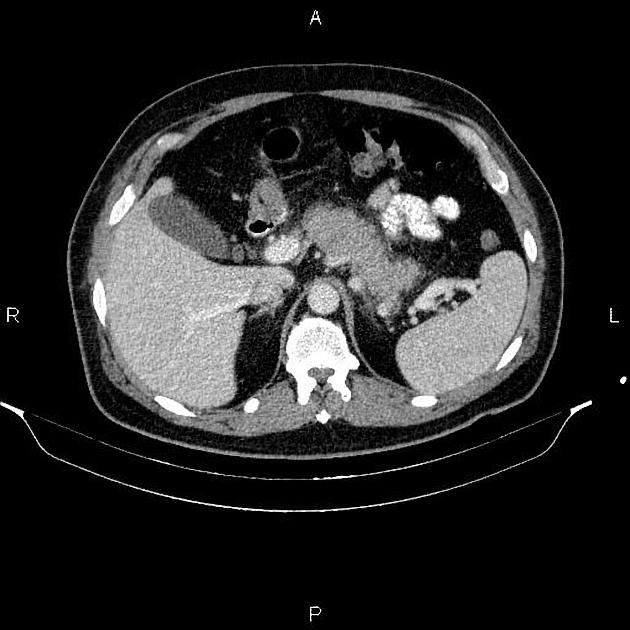
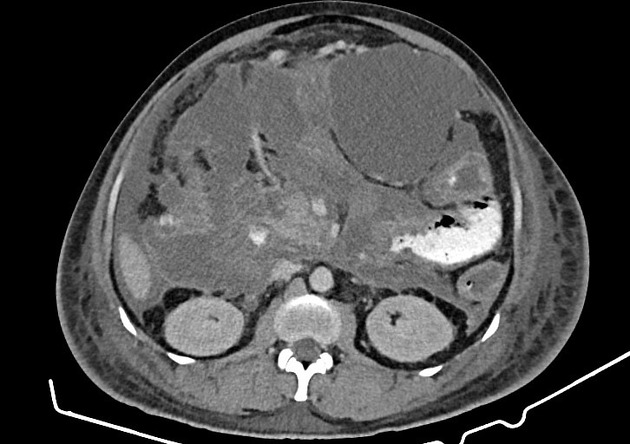
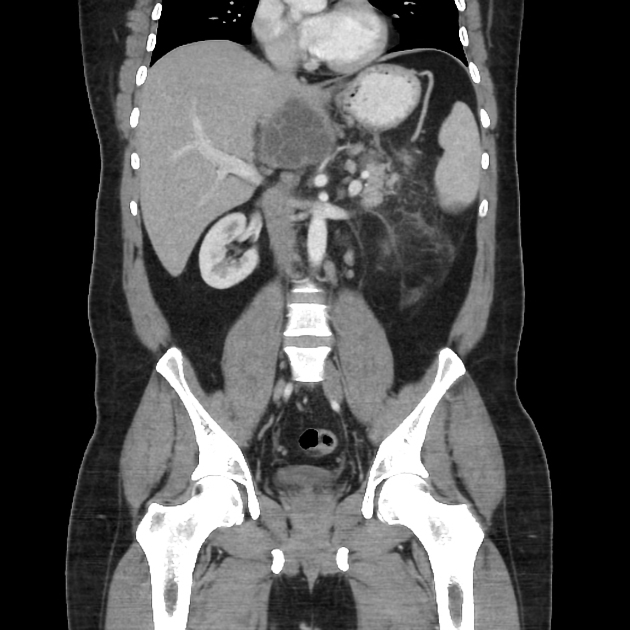
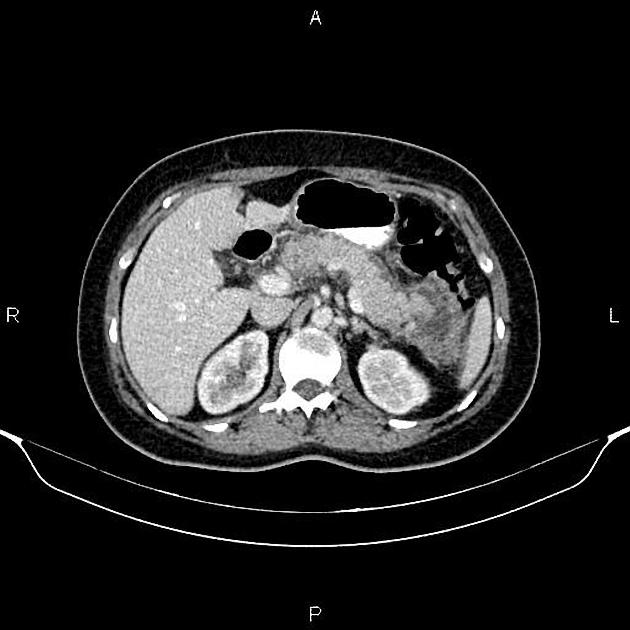
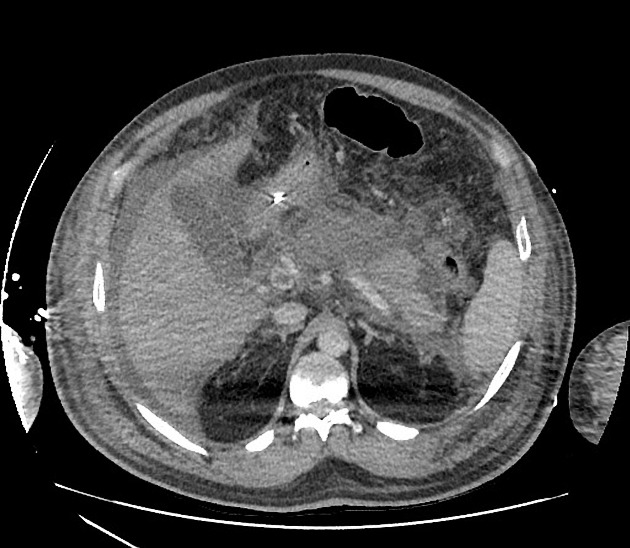
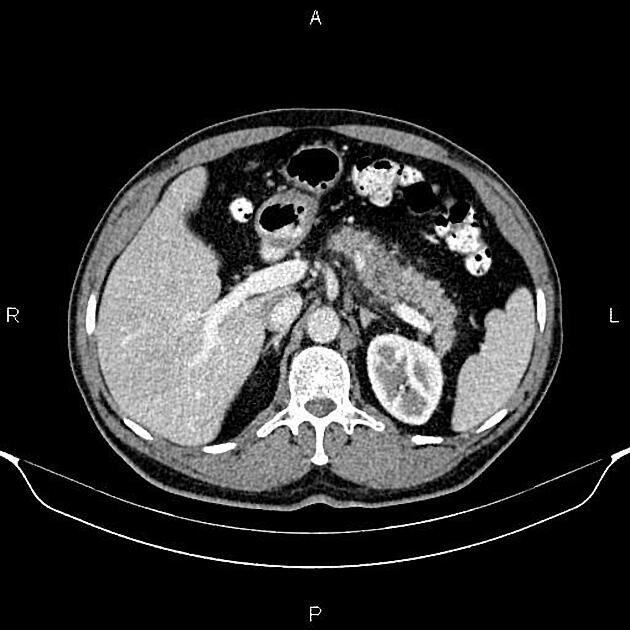
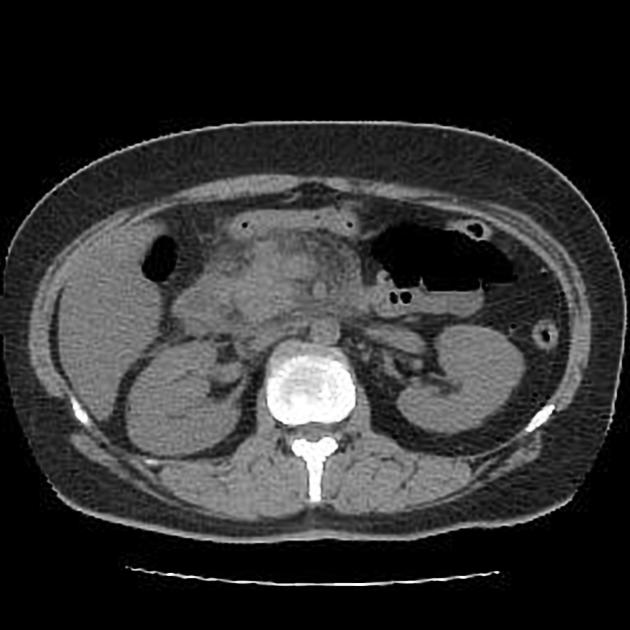
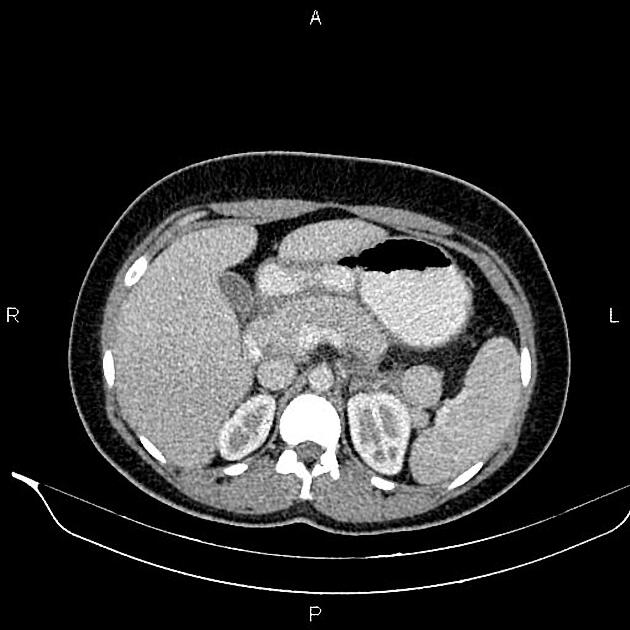
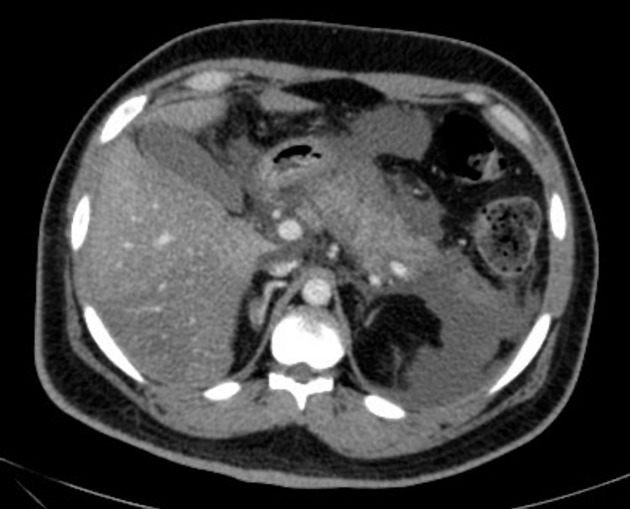
CT
Abnormalities that may be seen in the pancreas include:
-
typical findings
focal or diffuse parenchymal enlargement
changes in density because of edema
indistinct pancreatic margins owing to inflammation
surrounding retroperitoneal fat stranding
-
liquefactive necrosis of pancreatic parenchyma
lack of parenchymal enhancement (should ideally be 1 week after symptom onset to differentiate from pancreatic hypoenhancement secondary only to edema)
often multifocal
-
infected necrosis
difficult to distinguish from aseptic liquefactive necrosis
the presence of gas is helpful (emphysematous pancreatitis)
FNA helpful
-
abscess formation
circumscribed fluid collection
little or no necrotic tissues (thus distinguishing it from infected necrosis)
-
hemorrhage
high-attenuation fluid in the retroperitoneum or peripancreatic tissues
-
calcification
evidence of background chronic pancreatitis
-
retroperitoneal fat necrosis 33
low density collection showing minimal heterogeneity
mimicking carcinomatosis
Dual-energy CT
Dual-energy CT may be able to help better differentiate necrotic debris, hematoma, and areas of viable tissue in cases of necrotizing pancreatitis. In hemorrhagic pancreatitis, virtual non-contrast images can depict hematoma and differentiate it from parenchymal enhancement on contrast-enhanced images. It also improves the detection of non-calcified gallstones and isoattenuating cholesterol stones which may be the causative factor in the patient's pancreatitis 21.
Dual-energy CT dual-phase protocols with virtual non-contrast reformats can also offer lower radiation doses than conventional triple-phase CT imaging of the pancreas 21.
Grading of severity
CT is used to grade the severity of pancreatitis, following scoring systems can be used:
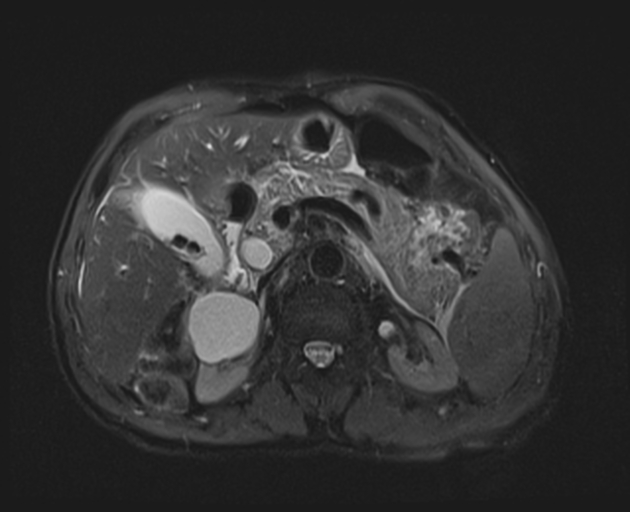
MRI
Contrast-enhanced MR is equivalent to CT in the assessment of acute pancreatitis.
Diffusion-weighted imaging shows hyperintense signal of the involved parenchyma with decreased ADC values 28,29.
Treatment and prognosis
Treatment is largely supportive, often requiring ICU care in severe cases for respiratory and cardiovascular support and careful management of glucose, calcium, and fluid balance.
Recommendations include 11:
aggressive fluid resuscitation in the first 24 hours
no need for prophylactic antibiotics
enteral feeding strongly preferred over parenteral feeding, especially in severe acute pancreatitis
no need for ERCP in acute gallstone pancreatitis unless evidence of ascending cholangitis
image-directed catheter placement is an alternative to surgical drainage of pancreatic fluid collections
cholecystectomy before discharge in patients with acute pancreatitis and gallstones found on imaging
The prognosis for acute pancreatitis varies according to severity. Overall mortality is 5-10% per attack 3. Various scoring systems exist that attempt to stratify severity (e.g. Ranson's criteria and APACHE II).
The 2012 revised Atlanta classification attempts to establish uniformity in reporting for both clinical practice and research 8.
Differential diagnosis
General imaging differential considerations include:
peptic ulcer disease with posterior perforation
pancreatic lymphoma (diffuse pattern)




















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.