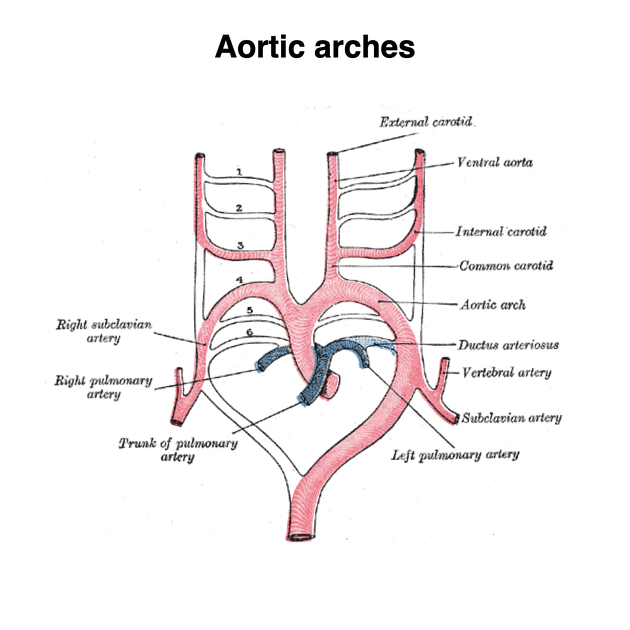
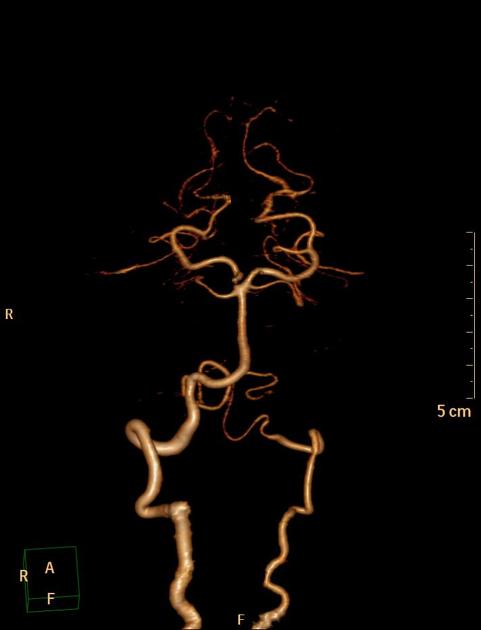
The vertebral arteries (VA) are paired arteries, each arising from the respective subclavian artery and ascending in the neck to supply the posterior fossa and occipital lobes, as well as provide segmental vertebral and spinal column blood supply.
On this page:
Summary
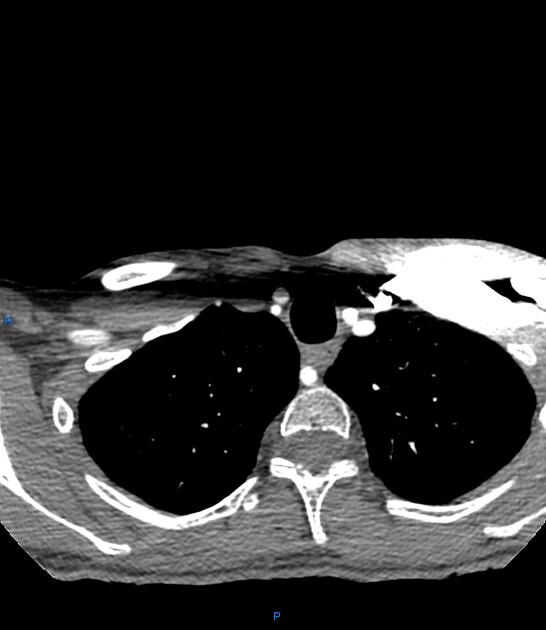
origin: branches of the 1st part of the subclavian artery
course: ascends posterior to the internal carotid artery in the transverse foramina of the cervical vertebrae
-
branches
numerous small branches
radicular/spinal branches
termination: combines with the contralateral vertebral artery to form the basilar artery
key relationships: posterior to the internal carotid artery; ascends anterior to the roots of the hypoglossal nerve (CN XII)
Gross anatomy
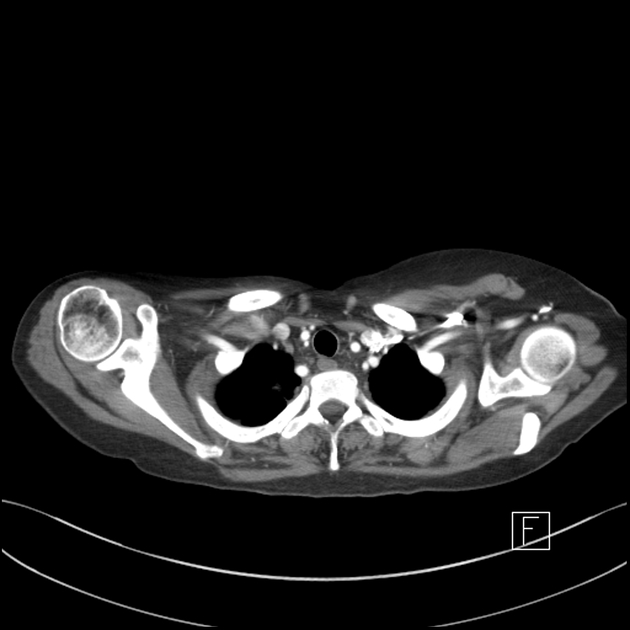
Origin
The origin of the vertebral arteries is usually from the posterior superior part of the subclavian arteries bilaterally, although the origin can be variable:
brachiocephalic artery (on the right)
aortic arch: 6% of cases, most on the left
The VA is normally 3-5 mm in diameter and the ostium is the most common site of stenosis.
When the origin is from the arch, then it is common for the artery to enter the foramen transversarium at a level higher than normal (C5 instead of C6).
Rarely, the right vertebral artery can have an aberrant origin distal to the left subclavian; see vertebral arteria lusoria.
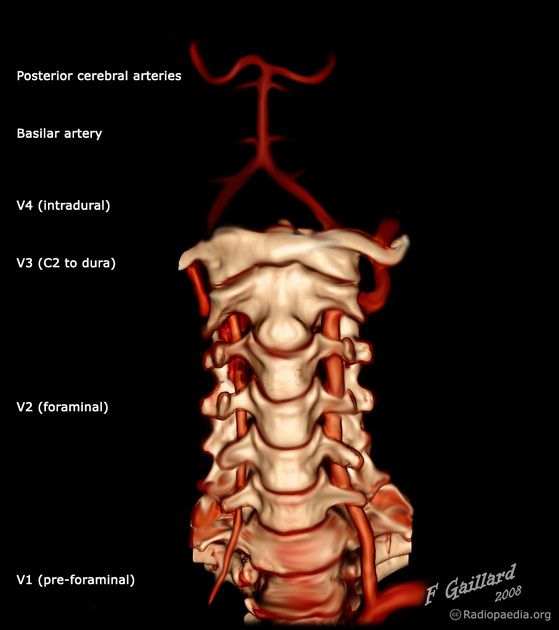
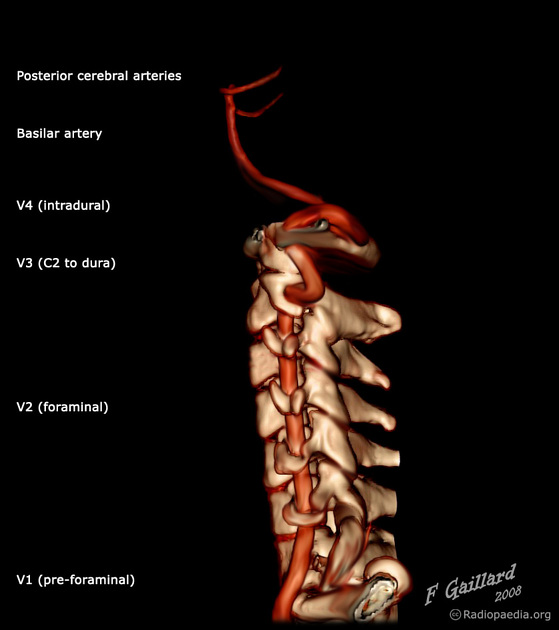
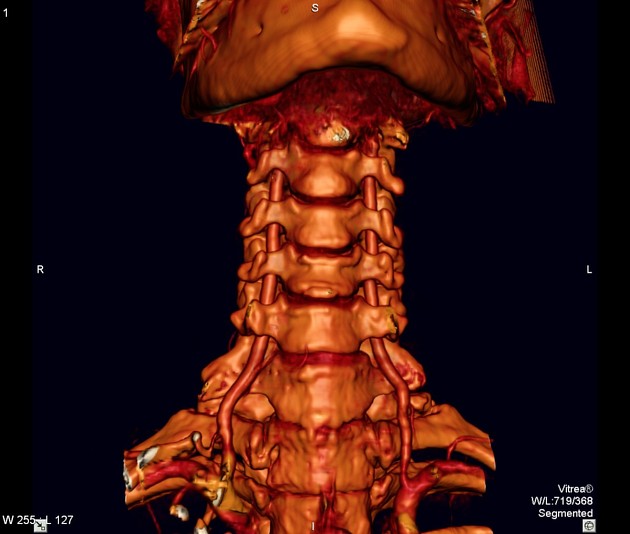
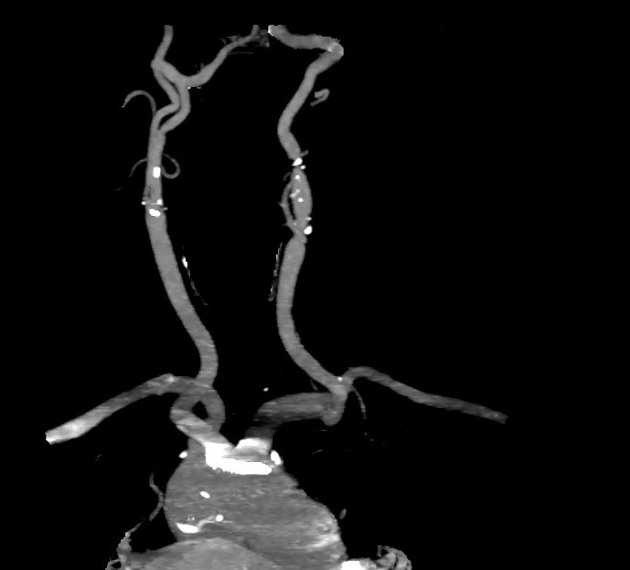
Segments
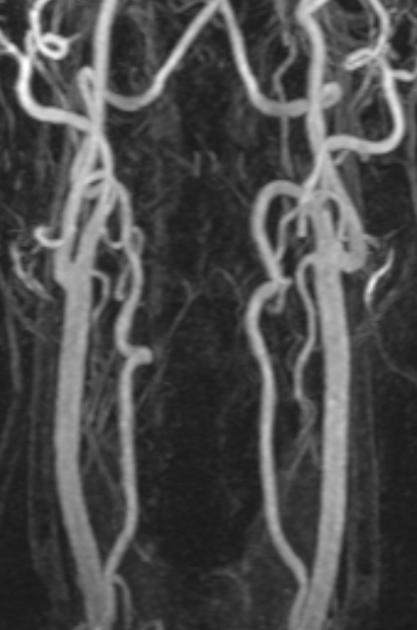
The vertebral artery is typically divided into 4 segments:
-
V1: pre-foraminal segment
origin to the transverse foramen of C6
-
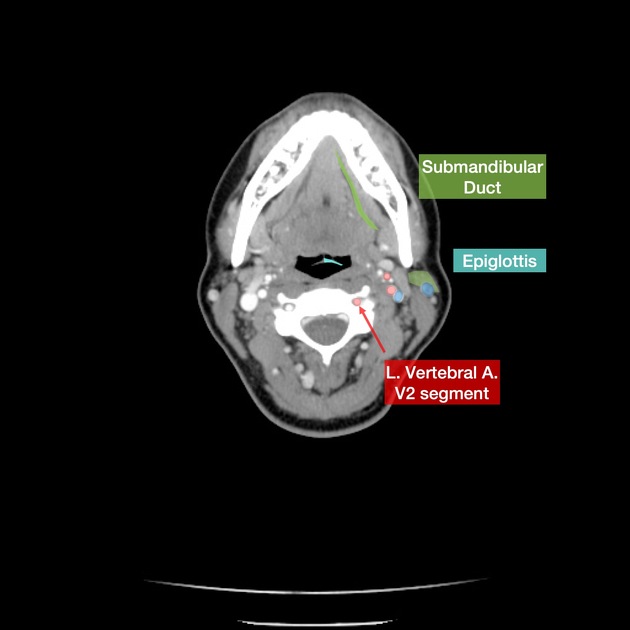
V2: foraminal segment
from the transverse foramen of C6 to the transverse foramen of C2
-
V3: atlantic, extradural or extraspinal segment
starts from C2, where the artery loops and turns lateral to ascend into the transverse foramen
continues through C1 to pierce the dura
-
V4: intradural or intracranial segment
from the dura at the lateral edge of the posterior atlanto-occipital membrane to their confluence on the medulla to form the basilar artery
Course
V1 (pre-foraminal)
Also known as the extraosseous segment, V1 arises from the first part of the subclavian artery. It angles posteriorly between longus colli medially and scalenus anterior laterally, through the colliscalene triangle, and behind the common carotid artery to enter the transverse foramen of C6.
Relations
anteriorly: common carotid artery, vertebral vein, thoracic duct (left VA), and lymphatic duct (right VA)
posteriorly: ventral rami of spinal nerves C7 and C8, transverse process of C7, inferior cervical ganglion
anteromedially: inferior thyroid artery, middle cervical ganglion
V2 (foraminal)
V2 ascends through the transverse foramina of the cervical vertebrae, normally C6-C3. Here it is accompanied by the vertebral veins and the sympathetic nerves. It then turns superolaterally through the inverted L-shaped transverse foramen of C2.
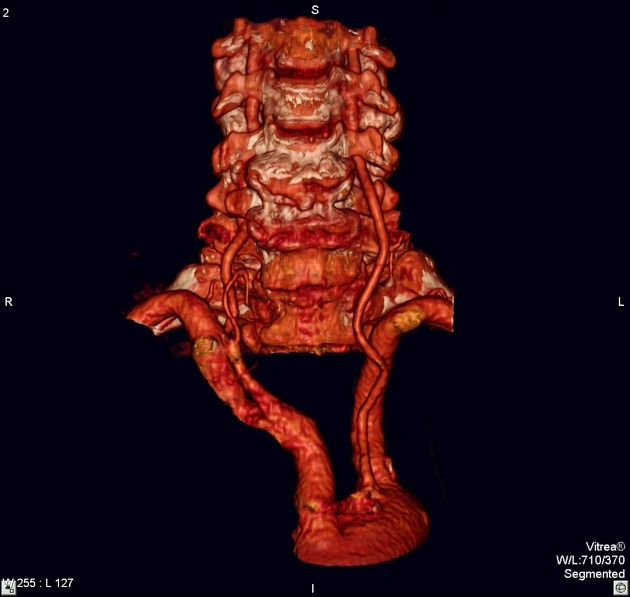
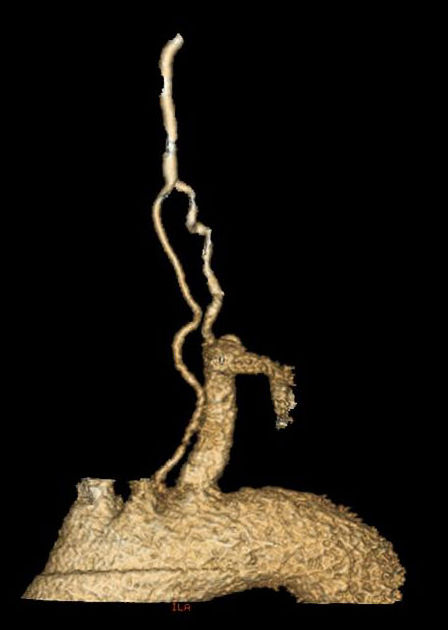
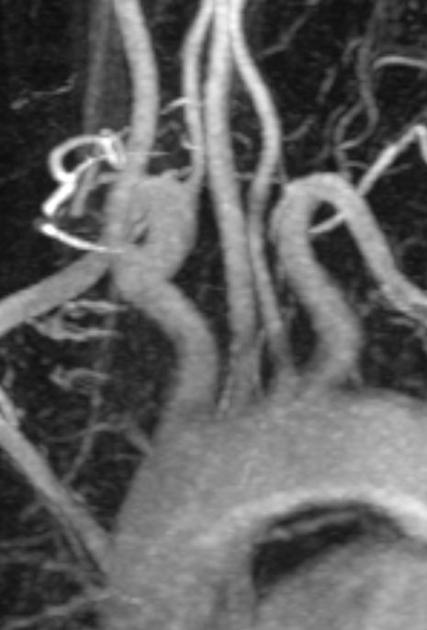
V3 (atlantic, extradural or extraspinal)
V3 ascends from the curved transverse foramen of C2 (axis) and sweeps laterally over the transverse process. It then curves superiorly passing immediately lateral to the lateral mass of C2 and the lateral C1/2 articulation before it passes through the transverse foramen of C1 (atlas). Exiting this foramen, V3 then once again courses posteriorly around the posterolateral border of the lateral mass of C1. Passing superomedially it grooves the upper surface of the posterior arch of C1 and will enter the spinal canal by piercing the posterior atlanto-occipital membrane, spinal dura and arachnoid to continue as V4. This tortuosity provides length and freedom for the vessel to stretch, straighten and bend during rotation of the head, which occurs at the atlanto-axial joints.
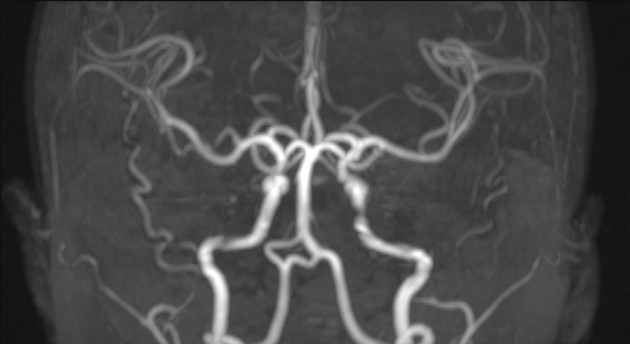
V4 (intradural or intracranial)
V4 ascends anterior to the roots of the hypoglossal nerve (CN XII) and joins its contralateral counterpart at the lower border of the pons to form the basilar artery.
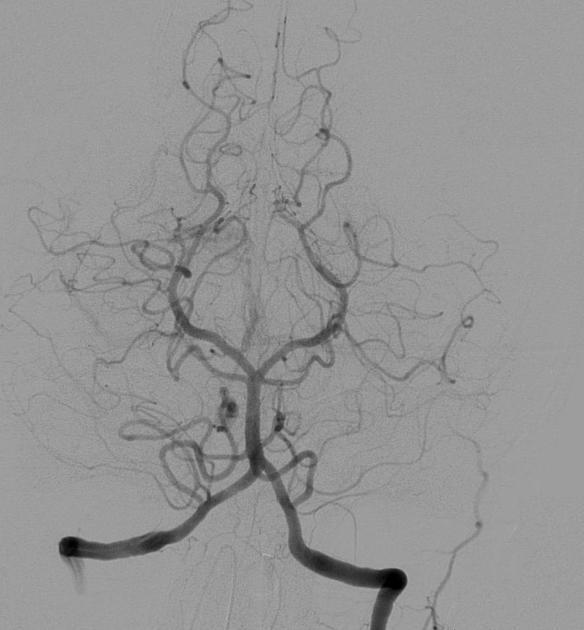
Branches
Numerous muscular branches are given off as the artery ascends, with relatively large ones passing posteriorly from V3 to supply the occipital triangle. They can anastomose with occipital branches of the ECA.
Spinal branches, pass into the spinal canal via the intervertebral foramina and contribute to supply not only of the vertebral bodies and extradural content of the canal but also of the dura and spinal cord, reinforcing the anterior and posterior spinal arteries.
The posterior inferior cerebellar artery (PICA) is the largest branch of the vertebral artery and is one of three main arteries supplying the cerebellum.
Other branches include:
V1: segmental cervical, muscular and spinal branches
V2: anterior meningeal artery, muscular and spinal branches
V4: anterior and posterior spinal arteries (ASA and PSA), perforating branches to medulla, posterior inferior cerebellar artery
Supply
ASA: upper cervical spinal cord, inferior medulla
PSA: dorsal spinal cord to conus medullaris
PICA: lateral medulla, tonsil, inferior vermis/cerebellum, choroid plexus of 4th ventricle
penetrating branches: portion of the medulla, olives, inferior cerebellar peduncle
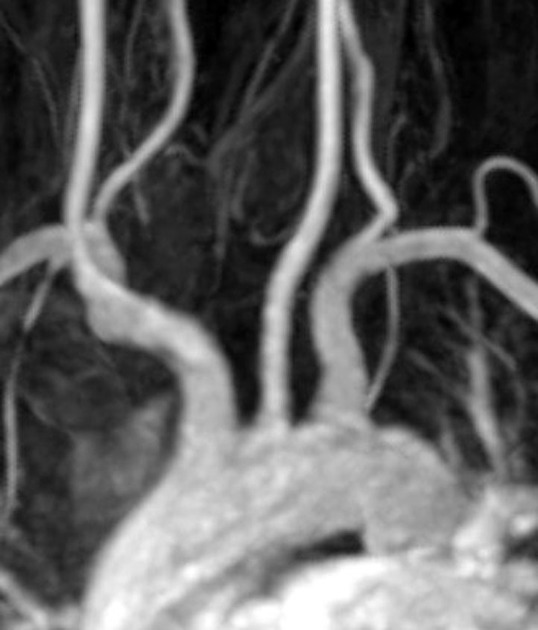
Variant anatomy
-
asymmetry due to vertebral arterial hypoplasia, absence or termination into PICA of one of the vertebral arteries is very common
left dominant ~45% (range 42-50%)
right dominant ~30% (range 25-32%)
co-dominant ~25% (range 25-26%)
complete or partial vertebral artery duplication
-
vertebral artery fenestration
incidence ~1% with extracranial fenestration more common than intracranial fenestration 17
increased association of intracranial aneurysms 17
-
variable origin
single left aberrant origin (86%), single right aberrant (12%), bilateral aberrant origin (3%) 8
aortic arch origin of the left vertebral artery: incidence ~5% (range 3.1-8.3%)
second (not first) branch of the subclavian artery
external carotid artery (rare) 8, 9
common carotid artery (rare) 9
internal carotid artery (rare) 9
origin from the distal aortic arch with an aberrant retro-oesophageal course (very rare) - see case 18
-
ostium may have a variable orientation
cranial ~47%
posterior ~45%
caudal ~5%
anterior ~3%
Ultrasound
peak velocities (PV) can have a wide range amongst individuals, ranging from 20-60 cm/s ref
luminal diameter may increase slightly with age 12
there is contradicting data amongst different publications as to if and how resistance index (RI) changes with ageing 12-16














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.