Hepatic hemangiomas or hepatic venous malformations are the most common benign vascular liver lesions. They are frequently diagnosed as an incidental finding on imaging, and most patients are asymptomatic. From a radiologic perspective, it is important to differentiate hemangiomas from hepatic malignancy.
On this page:
Terminology
It is important to note that according to newer nomenclature, these lesions are known as venous malformations (ISSVA classification of vascular anomalies) 20. Having said that, it is probably helpful to include the word 'hemangioma' in reports, as this term is ubiquitous in the literature and more familiar to many clinicians. The remainder of this article uses the terms 'hepatic hemangioma' and 'hepatic venous malformation' interchangeably.
Epidemiology
Hepatic hemangiomas are much more common in females, with an F:M of up to 5:1 17. They are rarely seen in young children, but infantile hepatic hemangioma is the most common, benign hepatic vascular tumor in infants.
Associations
extrahepatic hemangiomata
hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)
Kasabach-Merritt syndrome: with giant hemangiomas
Pathology
Hepatic hemangiomas are thought to be congenital in origin, non-neoplastic, and are almost always of the cavernous subtype. Blood supply is predominantly hepatic arterial, similar to other liver tumors. A peripheral location within the liver is most common 3.
Although more classically associated with hepatic adenomas, there is also believed to be a link between high estrogen states (pregnancy, exogenous intake) and increased size/number of hepatic hemangiomas 24.
Subtypes
typical hepatic hemangioma
-
atypical hepatic hemangioma 9,12
flash filling hepatic hemangioma: up to 16% of all hepatic hemangiomas
-
other unusual imaging patterns
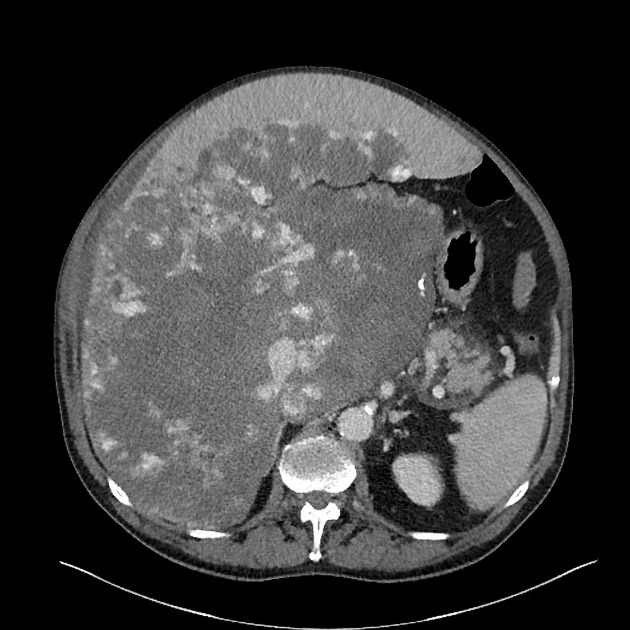
The presence of a few hepatic hemangiomas in the liver is not uncommon, but rarely a large number of hepatic hemangiomas may occur (see hepatic haemangiomatosis).
Radiographic features
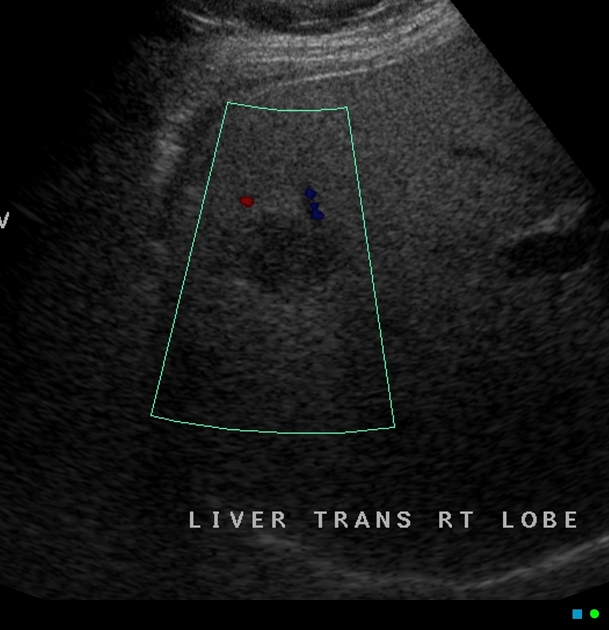
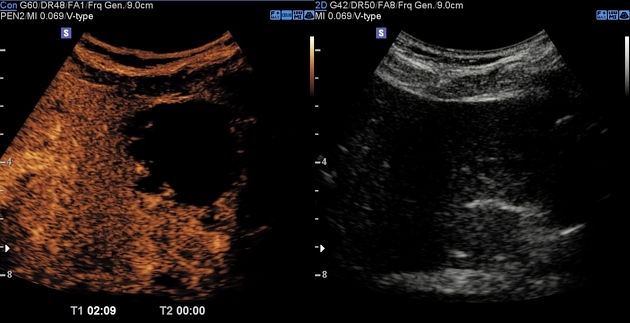
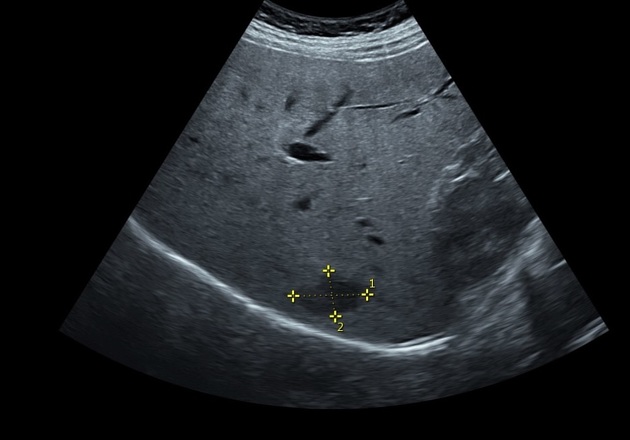
Ultrasound
typically well-defined hyperechoic lesions
a small proportion (10%) are hypoechoic, which may be due to a background of hepatic steatosis, where the liver parenchyma itself is of increased echogenicity
color Doppler: may show peripheral feeding vessels
-
contrast-enhanced ultrasound
arterial phase: peripheral nodular discontinuous enhancement
portal venous and delayed phases: continued "filling in" of the lesion, until the entire hemangioma is hyperechoic relative to background liver
central hemorrhagic portions of cavernous hemangiomas remain non-enhancing
See hyperechoic liver lesions for a further differential.
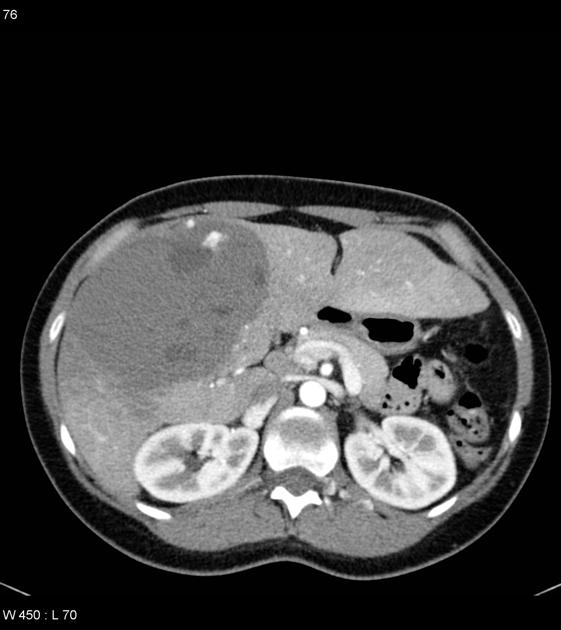
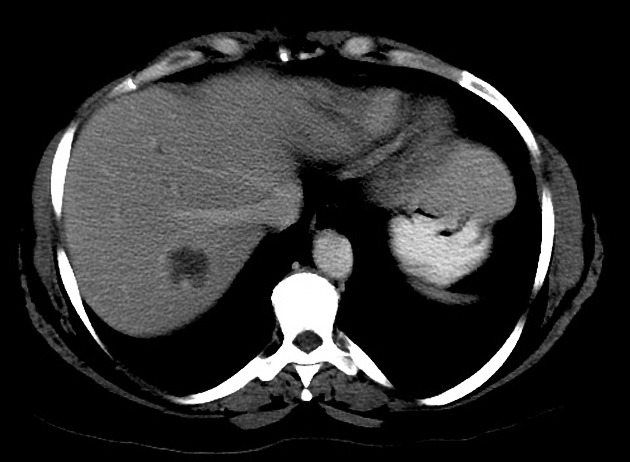
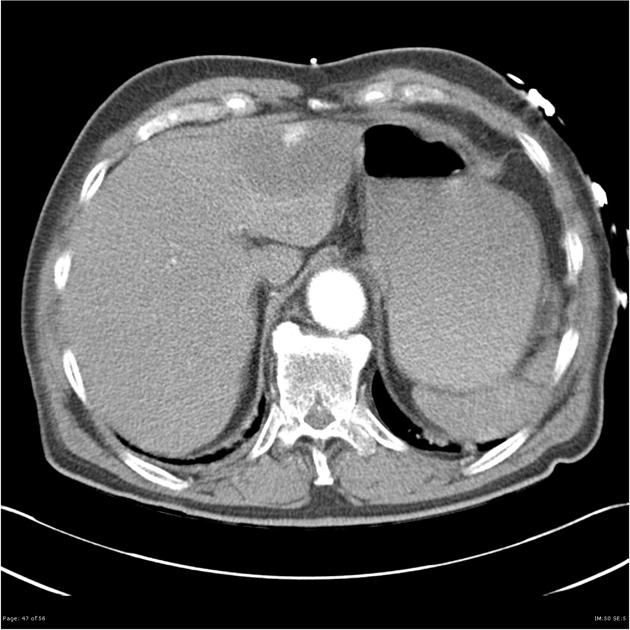
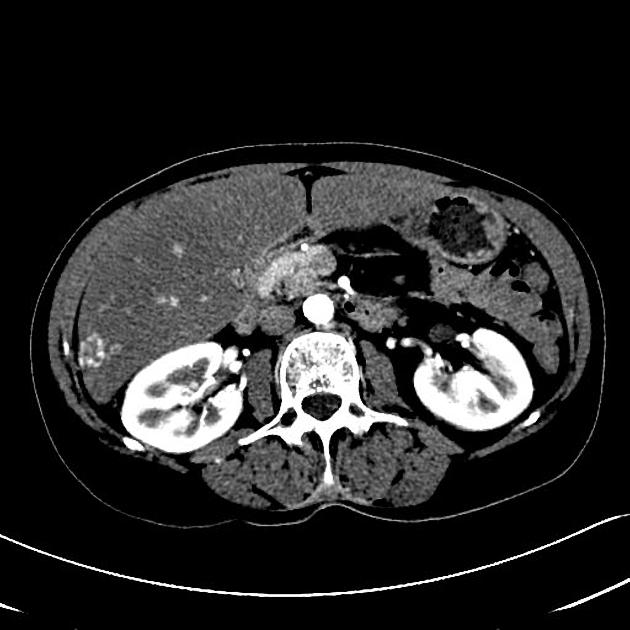
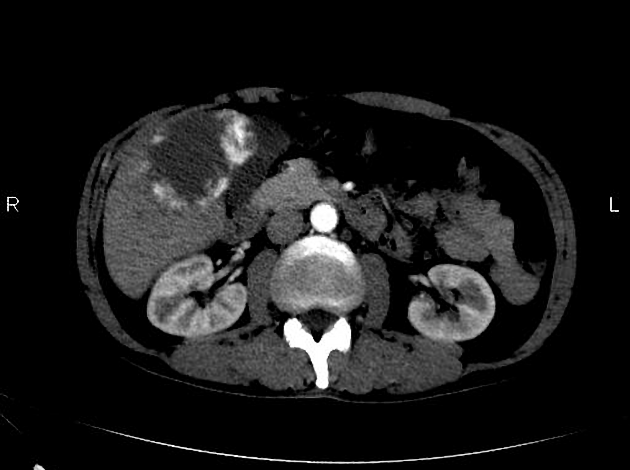
CT
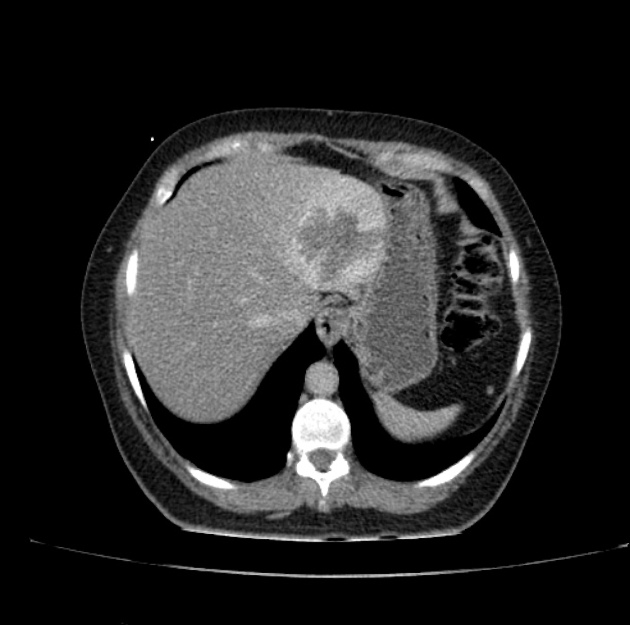
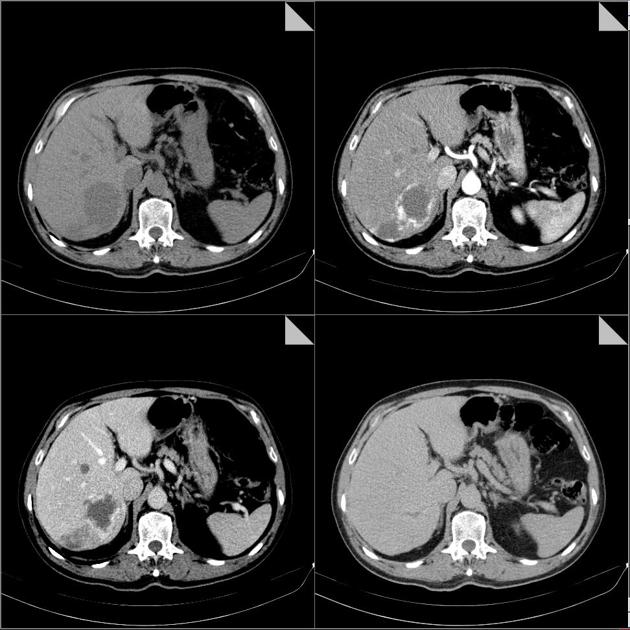
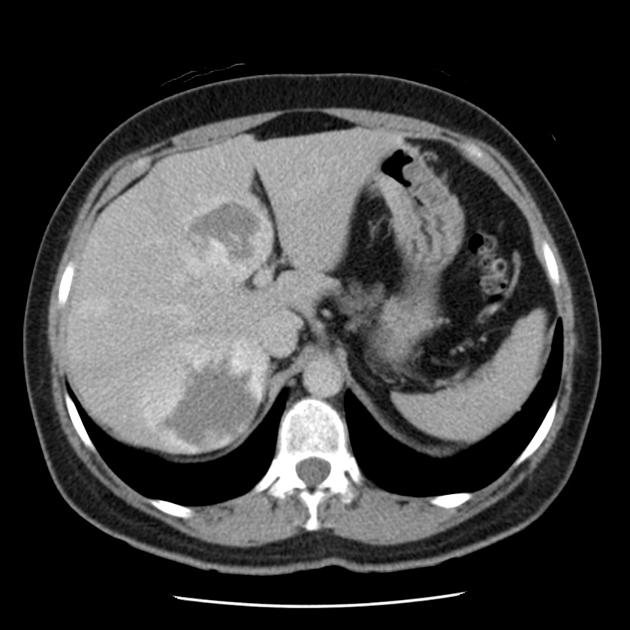
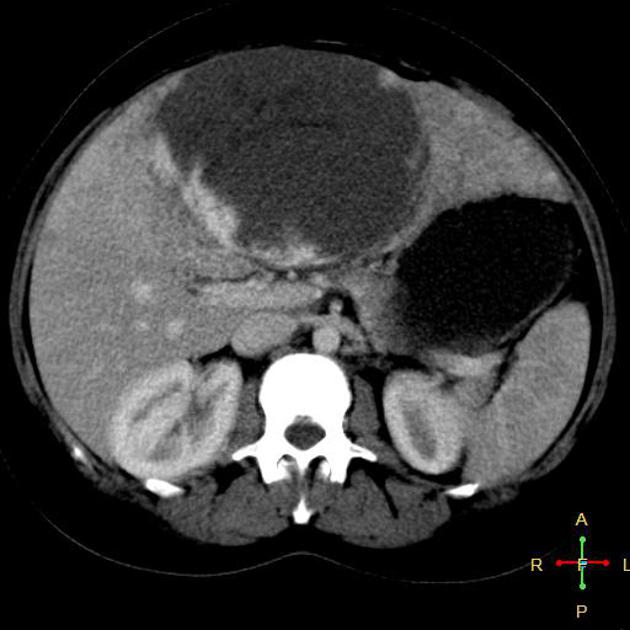
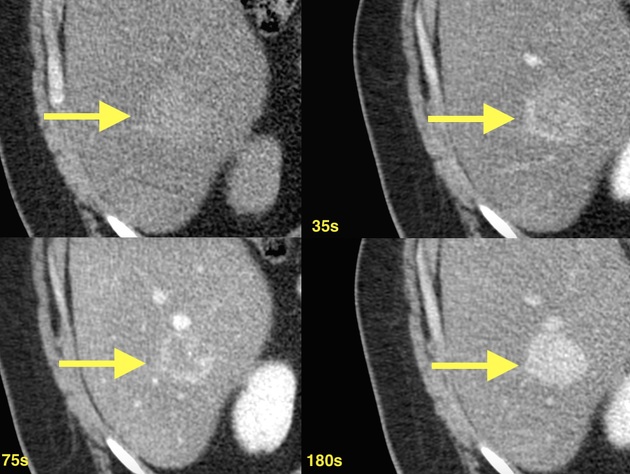
Most hemangiomas are relatively well-defined. The dynamic enhancement pattern is related to the size of its vascular space 1. Features of typical lesions include:
non-contrast: Often homogeneous hypoattenuating (<20 Hounsfield units) relative to liver parenchyma 23
late arterial phase: typically show discontinuous, nodular, peripheral enhancement (small lesions may show uniform enhancement)
portal venous phase: progressive peripheral enhancement with more centripetal fill-in
delayed phase: further irregular fill-in and therefore iso- or hyper-attenuating to liver parenchyma
Other described features include:
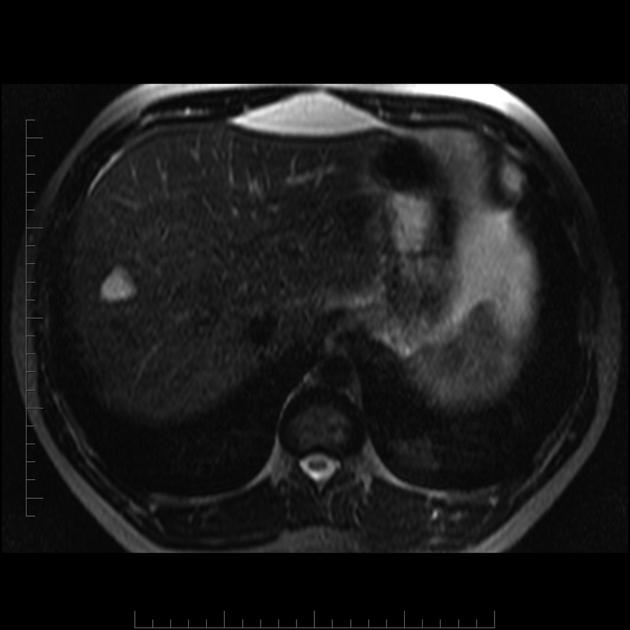
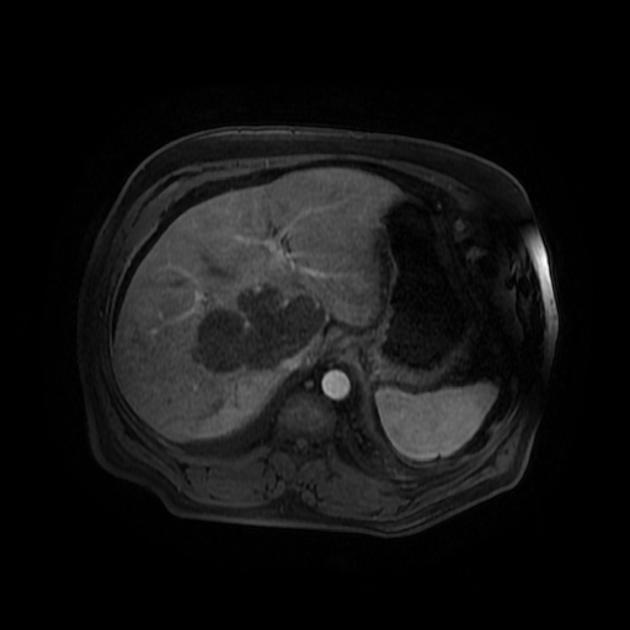
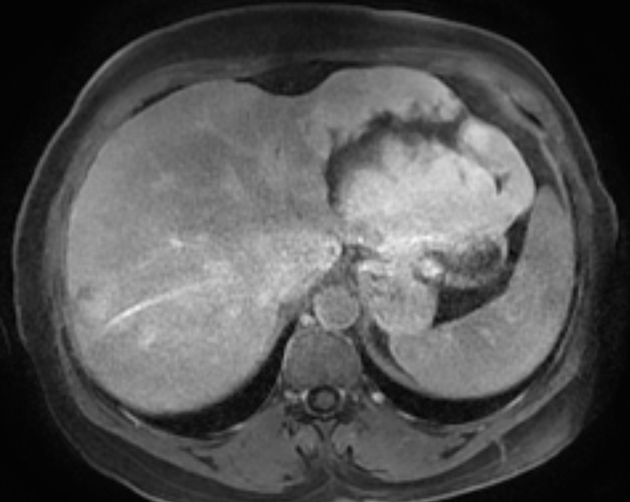
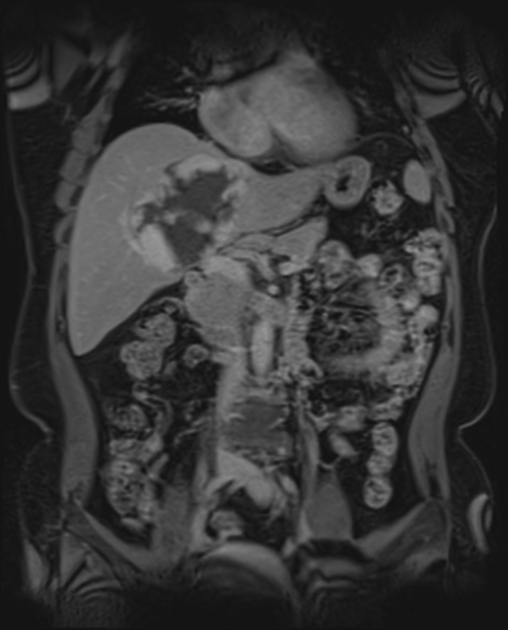
MRI
Typical features include:
T1: hypointense relative to liver parenchyma
T2: hyperintense relative to liver parenchyma, but less than the intensity of CSF or of a hepatic cyst
-
T1 C + (Gd): often shows peripheral nodular discontinuous enhancement which progresses centripetally (inward) on delayed images
hemangiomas tend to retain contrast on delayed (>5 minutes) contrast-enhanced images
atypical hemangiomas may demonstrate slightly altered enhancement patterns
-
T1 C + (hepatobiliary contrast, Eovist):
hemangiomas show a wide range of appearances on delayed imaging so this is less useful
high-flow hemangiomas may show 'pseudo washout' 21 - this is thought to be due to increased contrast uptake from the adjacent liver parenchyma and should not be confused with true washout
DWI: hyperintense on diffusion-weighted imaging even with high b-values due to slow blood flow and can be hyperintense or mixed (hyper and hypointense regions) on ADC map 16
Nuclear medicine
SPECT
Tc-99m RBCs labeled SPECT can be sensitive for larger lesions and typically demonstrate decreased activity on initial dynamic images followed by increased activity on delayed, blood pool images.
Treatment and prognosis
They are benign lesions. Recommendations for patients with no known risk factors for hepatic malignancy can range from center to center from performing confirmatory examinations (MRI, triphasic CT or scintigraphy) to considering follow-up ultrasound in 6 months to confirm stability, to performing no further imaging evaluation 13.
Some authors propose surgical resection for patients with progressive abdominal pain in combination with a size greater than 5 cm 14.
Differential diagnosis
The diagnosis of hemangioma can usually be made with high specificity if the imaging characteristics are typical. General imaging differential considerations for a hemangioma depend on the imaging modality and the patient's history, but may include:
focal hepatic steatosis: geographic hyperechoic lesion without mass effect or distortion of vessels (ultrasonography), requires dynamic phase CT or MRI for differentiation
hepatic metastases: hypervascular hepatic metastases show marked early enhancement with a continuous ring that on later images fills in centrally and progressive centripetal fill-in may occur on delayed phases 11
hepatic cyst: small lesions (generally <1 cm) on CT may be equivocal and can be clarified with a targeted ultrasound examination
cystic hepatic or biliary neoplasm


















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.