Polycystic ovaries (PCO) or polycystic ovarian morphology (PCOM) is an imaging descriptor of a particular type of change in ovarian morphology. A proportion of women with polycystic ovaries will have polycystic ovarian syndrome (PCOS), which in turn requires additional clinical, as well as biochemical, criteria; otherwise, polycystic ovaries can be considered a normal variant.
On this page:
Epidemiology
Polycystic ovaries may be seen in ~20% of women of reproductive age 1,4.
Radiographic features
Ultrasound
Transvaginal ultrasound is considered the gold standard in the diagnosis of polycystic ovarian morphology (although not in adolescents 18). Features can affect either one (unilateral polycystic ovary) or both ovaries.
Features include:
increased follicle number per ovary (FNPO): ≥20
background ovarian enlargement (volume greater than 10 mL) excluding dominant follicle >10 mm or corpus luteum 7
10 antral follicles of 2-9 mm or more per slice (FNPS): ≥10
individual follicles are generally similar in size and measure 2-9 mm in diameter 7
peripheral distribution of follicles; this can give a "string of pearls" appearance
central stromal brightness +/- prominence (increased ovarian stromal area to total ovarian area (S/A) ratio 17)
Only one ovary fitting these criteria is sufficient to define PCOM. If there is evidence of a dominant follicle (>10 mm) or a corpus luteum, the scan should be repeated during the next cycle 9.
The international PCOS consensus statement (2023) defines FNPO as 20 or more follicles per ovary 15, though earlier publications had suggested a more conservative cut-off of 25 follicles 14. It is now generally accepted that the initial Rotterdam recommendation of 12 follicles per ovary warrants revision, based on limited initial evidence and advances in ultrasound technology allowing better visualization of small follicles.
A study published in 2013 suggested that the number of follicles in each ovary, the follicle number per ovary (FNPO) is a more sensitive and specific criterion for diagnosis of PCO, as compared with the numbers of follicles in cross-section, also known as follicle number per section (FNPS), or ovarian volume. This study showed an FNPO threshold of 26 follicles had a sensitivity of 85% and specificity of 94% when discriminating between controls and PCOS. An FNPS threshold of nine follicles had a 69% sensitivity and 90% specificity, and an ovarian volume of 10 mL had an 81% sensitivity and 84% specificity 11.
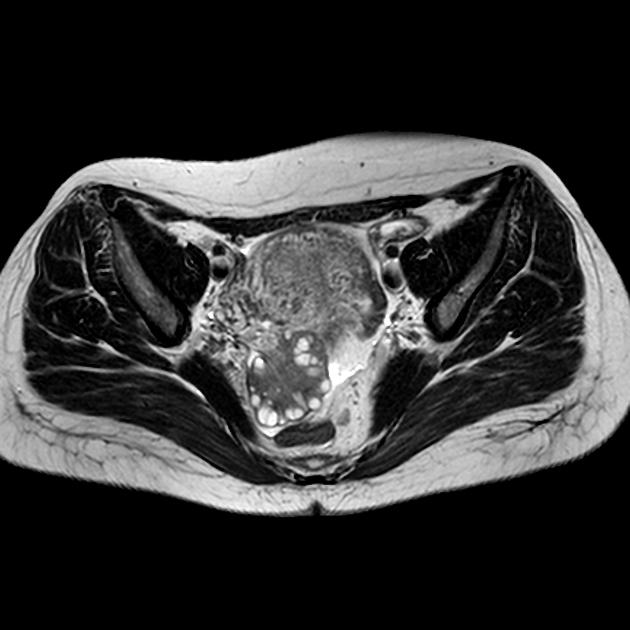
MRI
Pelvic MRI may show most or all of the above sonographic features. Signal characteristics include:
T1: small uniform follicles are low in signal while the central stroma is of intermediate signal (vs normal myometrium)
T2: follicles have high T2 signal while the central stroma is of comparatively low T2 signal 8
Differential diagnosis
General imaging differential considerations include:
multi-follicular ovaries (MFO): fewer cysts (~6 or more per ovary), which tend to be larger (up to 10 mm in diameter) and distributed throughout the ovary with no stromal hypertrophy 2
Practical points
TV imaging is preferable to TA imaging
only criteria (FNPO >20, ovarian volume >10 mL , FNPS >10) are required for the diagnosis of PCOM
PCOM can be seen without clinical manifestations of PCOS








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.