Extraprostatic extension of prostate cancer
Citation, DOI, disclosures and article data
At the time the article was created Paresh K Desai had no recorded disclosures.
View Paresh K Desai's current disclosuresAt the time the article was last revised Jeremy Jones had no recorded disclosures.
View Jeremy Jones's current disclosures- Prostate cancer: extracapsular extension
- Prostate carcinoma: extracapsular extension
- Extracapsular extension of prostate cancer
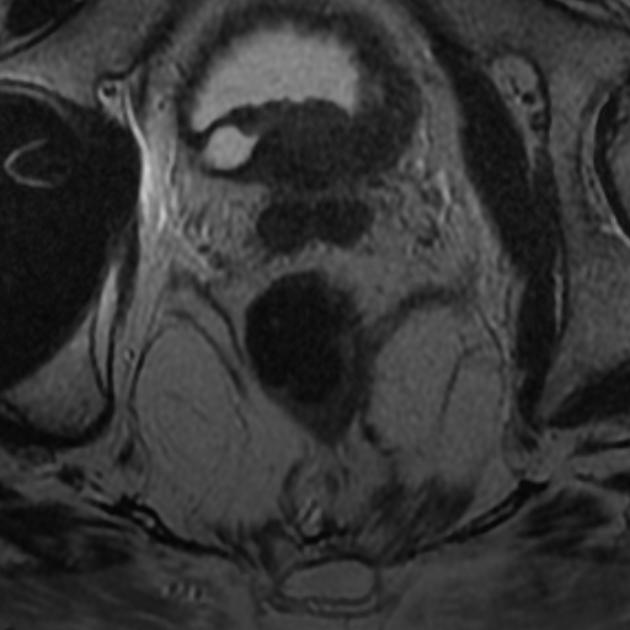
Extraprostatic (extracapsular) extension of prostate cancer refers to local tumor growth beyond the fibromuscular pseudocapsule of the prostate gland into the periprostatic soft tissues, in particular, the periprostatic fat and is an established adverse prognostic factor and of importance for prostate cancer staging and therapy.
On this page:
Anatomy
The prostate gland lacks a true capsule and the so-called "prostate capsule" is a pseudocapsule formed from fibromuscular tissue surrounding three distinct layers of fascia; the anterior, lateral, and posterior fasciae. Anteriorly and apically this pseudocapsule is deficient. Laterally the fascia fuses with the levator fascia. The prostatic venous plexus (Santorini plexus) lies between and passes through, the pseudocapsule and fascia 10-13.
Radiographic features
Though imperfect, MRI is superior to transrectal ultrasound, CT, and digital rectal examination in predicting the likelihood of extracapsular extension.
MRI
Morphologic predictors of extraprostatic extension at MRI are listed in rough order from most specific to most sensitive 1,3,4:
- seminal vesicle invasion (asymmetric loss of normal high T2 signal in the seminal vesicular lumen)
- neurovascular asymmetry (unequal appearance of neurovascular bundles when an ipsilateral tumor is present)
- frank capsular breach (tumor clearly extends into the periprostatic fat or invades adjacent organs such as rectum or bladder)
- obliteration of the rectoprostatic angle (loss of fatty space between prostate and rectum; posteriorly located tumors only)
- capsular bulge (smooth or irregular convex outward protrusion of prostate margin continuous with the tumor)
- broad capsular contact (≥10-20 mm in a curvilinear length of contact between tumor and capsule) 1,5-7
Independent of these morphological criteria, the risk of extraprostatic extension also correlates with the PI-RADS assessment category on multiparametric MRI (mpMRI) 9.
Treatment and prognosis
On preoperative imaging, the suggestion of extraprostatic extension is important for surgical planning and counseling as resection of the neurovascular bundle may be required.
Extraprostatic extension is associated with a higher risk of recurrence and metastasis and lower cancer-specific survival after radical prostatectomy 1.
See also
References
- 1. Mehralivand S, Shih JH, Harmon S, Smith C, Bloom J, Czarniecki M, Gold S, Hale G, Rayn K, Merino MJ, Wood BJ, Pinto PA, Choyke PL, Turkbey B. A Grading System for the Assessment of Risk of Extraprostatic Extension of Prostate Cancer at Multiparametric MRI. (2019) Radiology. 290 (3): 709-719. doi:10.1148/radiol.2018181278 - Pubmed
- 2. Mullerad M, Hricak H, Wang L et-al. Prostate cancer: detection of extracapsular extension by genitourinary and general body radiologists at MR imaging. Radiology. 2004;232 (1): 140-6. doi:10.1148/radiol.2321031254 - Pubmed citation
- 3. Bonekamp D, Jacobs MA, El-Khouli R et-al. Advancements in MR imaging of the prostate: from diagnosis to interventions. Radiographics. 2011;31 (3): 677-703. doi:10.1148/rg.313105139 - Free text at pubmed - Pubmed citation
- 4. Yu KK, Hricak H, Alagappan R et-al. Detection of extracapsular extension of prostate carcinoma with endorectal and phased-array coil MR imaging: multivariate feature analysis. Radiology. 1997;202 (3): 697-702. Radiology (abstract) - Pubmed citation
- 5. Rosenkrantz AB, Shanbhogue AK, Wang A, Kong MX, Babb JS, Taneja SS. Length of capsular contact for diagnosing extraprostatic extension on prostate MRI: Assessment at an optimal threshold. (2016) Journal of magnetic resonance imaging : JMRI. 43 (4): 990-7. doi:10.1002/jmri.25040 - Pubmed
- 6. Krishna S, Lim CS, McInnes MDF, Flood TA, Shabana WM, Lim RS, Schieda N. Evaluation of MRI for diagnosis of extraprostatic extension in prostate cancer. (2018) Journal of magnetic resonance imaging : JMRI. 47 (1): 176-185. doi:10.1002/jmri.25729 - Pubmed
- 7. Baco E, Rud E, Vlatkovic L, Svindland A, Eggesbø HB, Hung AJ, Matsugasumi T, Bernhard JC, Gill IS, Ukimura O. Predictive value of magnetic resonance imaging determined tumor contact length for extracapsular extension of prostate cancer. (2015) The Journal of urology. 193 (2): 466-72. doi:10.1016/j.juro.2014.08.084 - Pubmed
- 8. Fütterer JJ, Heijmink SW, Scheenen TW, Jager GJ, Hulsbergen-Van de Kaa CA, Witjes JA, Barentsz JO. Prostate cancer: local staging at 3-T endorectal MR imaging--early experience. (2006) Radiology. 238 (1): 184-91. doi:10.1148/radiol.2381041832 - Pubmed
- 9. Kayat Bittencourt L, Litjens G, Hulsbergen-van de Kaa CA, Turkbey B, Gasparetto EL, Barentsz JO. Prostate Cancer: The European Society of Urogenital Radiology Prostate Imaging Reporting and Data System Criteria for Predicting Extraprostatic Extension by Using 3-T Multiparametric MR Imaging. (2015) Radiology. 276 (2): 479-89. doi:10.1148/radiol.15141412 - Pubmed
- 10. Lee CH, Akin-Olugbade O, Kirschenbaum A. Overview of prostate anatomy, histology, and pathology. (2011) Endocrinology and metabolism clinics of North America. 40 (3): 565-75, viii-ix. doi:10.1016/j.ecl.2011.05.012 - Pubmed
- 11. Chummy S. Sinnatamby. Last's Anatomy. (2020) ISBN: 9780702033957
- 12. Kiyoshima K, Yokomizo A, Yoshida T, Tomita K, Yonemasu H, Nakamura M, Oda Y, Naito S, Hasegawa Y. Anatomical features of periprostatic tissue and its surroundings: a histological analysis of 79 radical retropubic prostatectomy specimens. (2004) Japanese journal of clinical oncology. 34 (8): 463-8. doi:10.1093/jjco/hyh078 - Pubmed
- 13. Kundra V, Silverman PM, Matin SF, Choi H. Imaging in oncology from the University of Texas M. D. Anderson Cancer Center: diagnosis, staging, and surveillance of prostate cancer. (2007) AJR. American journal of roentgenology. 189 (4): 830-44. doi:10.2214/AJR.07.2011 - Pubmed
Incoming Links
- Prostate cancer (staging)
- Intraductal carcinoma of the prostate
- Prostate MRI protocol
- Mucinous adenocarcinoma of the prostate
- Small cell carcinoma of the prostate
- Squamous neoplasms of the prostate
- Seminal vesicle invasion
- Basal cell carcinoma of the prostate
- Prostate cancer
- Prostate Imaging-Reporting and Data System (PI-RADS)
- Prostate cancer
- Prostate cancer skeletal metastases - superscan
- Locally advanced prostate cancer
- Spinal cord compression from metastatic prostate cancer
- Prostate carcinoma (T4N1M1b)
- Prostate cancer - detected on TURP
- Prostate cancer - locally progressive (T3b)
- Prostate cancer - staging
- Prostate cancer - staging
- Prostate cancer - staging
- Prostate cancer - seminal vesicle invasion
- Prostate cancer - extraprostatic extension
- Prostate cancer - extraprostatic extension
- Prostate cancer (MR in-bore biopsy)
- Prostate-seminal vesicle angle (TRUS)
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta previa
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumors
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumors of the testis
- testicular seminoma
-
non seminomatous germ cell tumors
- mixed germ cell tumor
- yolk sac tumor (endodermal sinus tumor)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumor
- sex cord / stromal tumors of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumor of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumors (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumors
- ureteral trauma
- other
- bladder
- kidneys





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.