Polyorchidism
Citation, DOI, disclosures and article data
At the time the article was created Vasileios Rafailidis had no recorded disclosures.
View Vasileios Rafailidis's current disclosuresAt the time the article was last revised Jeremy Jones had no financial relationships to ineligible companies to disclose.
View Jeremy Jones's current disclosures- Triorchidism
- Supernumerary testes
- Supernumerary testis
- Supernumerary testicles
- Supernumerary testicle
Polyorchidism, also known as supernumerary testes, refers to the presence of more than two testes and is a very rare congenital anomaly. The supernumerary testis can be usually located inside the scrotum (75% of the patients) or less commonly in the inguinal canal, the retroperitoneum, or the abdominal cavity 1-3.
On this page:
Epidemiology
Polyorchidism is rare, with only 140 cases reported up to 2013.
Clinical presentation
Polyorchidism is asymptomatic in the majority of patients. Some patients may present with scrotal pain, scrotal swelling, hydrocele, varicocele, epididymitis, infertility, testicular malignancy, or testicular torsion 2. Testicular torsion is the most commonly encountered complication of polyorchidism 3.
Clinical examination usually reveals that the testes have normally descended into the scrotum. However, a nodule can be palpable inside the affected hemiscrotum. This nodule is easily differentiated from the normal testes but may raise concern for malignancy.
As polyorchidism usually causes no symptoms, it is often found incidentally during self-examination or surgery for inguinal hernia, testicular tumor, or torsion 1. Polyorchidism is commonly associated with inguinal hernia (24%), undescended testis (22%) and microlithiasis 1.
ADVERTISEMENT: Supporters see fewer/no ads
Pathology
There are several types of this condition with triorchidism being the most common. In this type, there are three testes with the supernumerary being situated on the left in 65% of the cases. In 4.3% of patients with polyorchidism, there is bilateral involvement with four testes.
Etiology
Polyorchidism is a developmental anomaly with abnormal division of the genital ridge. The genital ridge can be longitudinally or transversely divided or duplicated before the 8th week of fetal development. The Wolffian duct may be duplicated as well.
Classification
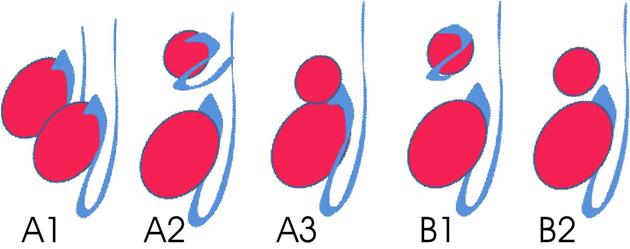
Polyorchidism is classified into two major types, A and B, based on the venous drainage of the testis (see Figure 1).
-
type A polyorchidism: the supernumerary testis is drained by a separate ductus deferens and consequently has reproductive potential
type A3 represents the most frequent subtype and represents 90% of all cases of polyorchidism
type B polyorchidism: the supernumerary testis is not drained by a ductus deferens and thus has no reproductive potential 1
ADVERTISEMENT: Supporters see fewer/no ads
Radiographic features
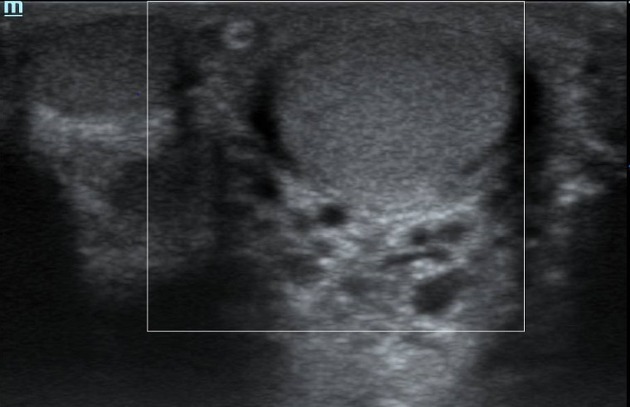
Ultrasound
Scrotal ultrasonography demonstrates the normal echogenicity of the testes. The supernumerary testis/testes can be seen as a solid nodule isoechoic to the testes and has the same echotexture. This nodule is usually located lower than the normal testes and is smaller. Hydrocele is present in 9% of patients 1.
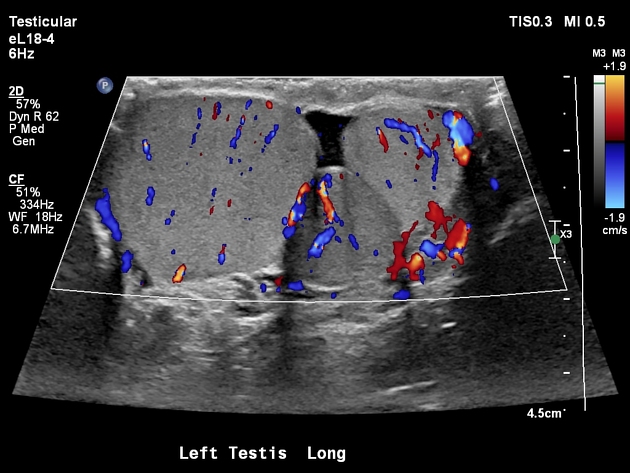
Color Doppler or power Doppler ultrasonography reveals normal blood flow in the supernumerary testis, with the same characteristics as in the two normal testes 4.
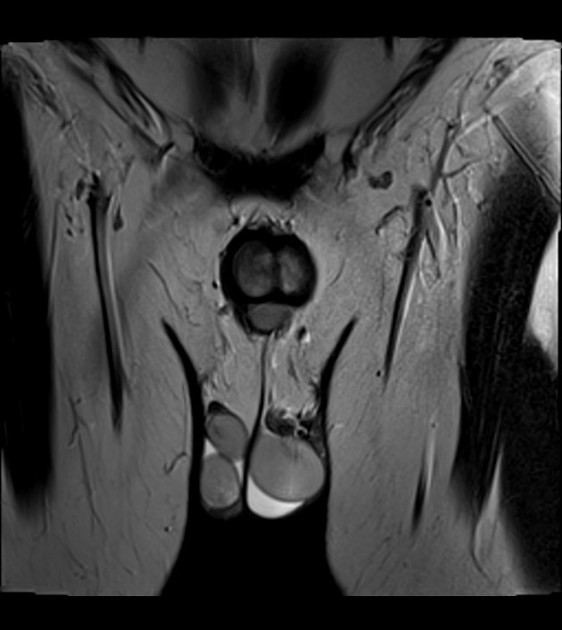
MRI
In case ultrasonography does not provide a conclusive diagnosis, MRI can be very helpful. The supernumerary testis has the same signal intensity as the normal testes 4:
T1: intermediate signal intensity
T2: high signal intensity
Treatment and prognosis
The management of patients with polyorchidism is under debate. Removal of a supernumerary or ectopic testis with orchiectomy is recommended by some due to the high risk of malignancy (4-7%). Cryptorchidism is considered to be the greatest risk factor for malignancy in patients presenting with polyorchidism.
Alternative management includes preservation of an incidentally found supernumerary testis and long-term follow-up. Treatment can be based on whether or not the supernumerary testis possesses a ductus deferens 2-4.
ADVERTISEMENT: Supporters see fewer/no ads
History and etymology
The term "polyorchidism" derives from the Greek root "πολυ-" (poly-) meaning plenty and the word "όρχις" (orchis) meaning testis and was first used by Arbuthnot Lane in 1895 to report a case discovered at surgery.
Differential diagnosis
Possible differential considerations include:
References
- 1. Alamsahebpour A, Hidas G, Kaplan A, McAleer I. Bilateral Polyorchidism with Diffuse Microlithiasis: A Case Report of an Adolescent with 4 Testes. Urology. 2013;82(6):1421-3. doi:10.1016/j.urology.2013.06.039 - Pubmed
- 2. Savas M, Yeni E, Ciftci H, Cece H, Topal U, Utangac M. Polyorchidism: A Three-Case Report and Review of the Literature. Andrologia. 2010;42(1):57-61. doi:10.1111/j.1439-0272.2009.00957.x - Pubmed
- 3. Bergholz R & Wenke K. Polyorchidism: A Meta-Analysis. J Urol. 2009;182(5):2422-7. doi:10.1016/j.juro.2009.07.063 - Pubmed
- 4. Arslanoglu A, Tuncel S, Hamarat M. Polyorchidism: Color Doppler Ultrasonography and Magnetic Resonance Imaging Findings. Clin Imaging. 2013;37(1):189-91. doi:10.1016/j.clinimag.2012.03.006 - Pubmed
- 5. Khedis M, Nohra J, Dierickx L et al. Polyorchidism: Presentation of 2 Cases, Review of the Literature and a New Management Strategy. Urol Int. 2008;80(1):98-101. doi:10.1159/000111738 - Pubmed
- 6. Oner A, Sahin C, Pocan S, Kizilkaya E. Polyorchidism: Sonographic and Magnetic Resonance Image Findings. Acta Radiol. 2005;46(7):769-71. doi:10.1080/02841850500216293 - Pubmed
- 7. Amodio J, Maybody M, Slowotsky C, Fried K, Foresto C. Polyorchidism: Report of 3 Cases and Review of the Literature. J Ultrasound Med. 2004;23(7):951-7. doi:10.7863/jum.2004.23.7.951 - Pubmed
- 8. Chintamani J, Nyapathy2 V, Chauhan3 A, Krishnamurthy4 U. Supernumerary Testis. J Radiol Case Rep. 2009;3(11):29-32. doi:10.3941/jrcr.v3i11.308 - Pubmed
Incoming Links
Related articles: Anatomy: Abdominopelvic
- skeleton of the abdomen and pelvis
- muscles of the abdomen and pelvis
- spaces of the abdomen and pelvis
- anterior abdominal wall
- posterior abdominal wall
- abdominal cavity
- pelvic cavity
- perineum
- abdominal and pelvic viscera
- gastrointestinal tract
- spleen
- hepatobiliary system
-
endocrine system
-
adrenal gland
- adrenal vessels
- chromaffin cells
- variants
- pancreas
- organs of Zuckerkandl
-
adrenal gland
-
urinary system
-
kidney
- renal pelvis
- renal sinus
- avascular plane of Brodel
-
variants
- number
- fusion
- location
- shape
- ureter
- urinary bladder
- urethra
- embryology
-
kidney
- male reproductive system
-
female reproductive system
- vulva
- vagina
- uterus
- adnexa
- Fallopian tubes
- ovaries
- broad ligament (mnemonic)
- variant anatomy
- embryology
- blood supply of the abdomen and pelvis
- arteries
-
abdominal aorta
- inferior phrenic artery
- celiac artery
- superior mesenteric artery
- middle suprarenal artery
- renal artery (variant anatomy)
- gonadal artery (ovarian artery | testicular artery)
- inferior mesenteric artery
- lumbar arteries
- median sacral artery
-
common iliac artery
- external iliac artery
-
internal iliac artery (mnemonic)
- anterior division
- umbilical artery
- superior vesical artery
- obturator artery
- vaginal artery
- inferior vesical artery
- uterine artery
- middle rectal artery
-
internal pudendal artery
- inferior rectal artery
-
perineal artery
- posterior scrotal artery
- transverse perineal artery
- artery to the bulb
- deep artery of the penis/clitoris
- dorsal artery of the penis/clitoris
- inferior gluteal artery
- posterior division (mnemonic)
- variant anatomy
- anterior division
-
abdominal aorta
- portal venous system
- veins
- anastomoses
- arterioarterial anastomoses
- portal-systemic venous collateral pathways
- watershed areas
- arteries
- lymphatics
- innervation of the abdomen and pelvis
- thoracic splanchnic nerves
- lumbar plexus
-
sacral plexus
- lumbosacral trunk
- sciatic nerve
- superior gluteal nerve
- inferior gluteal nerve
- nerve to piriformis
- perforating cutaneous nerve
- posterior femoral cutaneous nerve
- parasympathetic pelvic splanchnic nerves
- pudendal nerve
- nerve to quadratus femoris and inferior gemellus muscles
- nerve to internal obturator and superior gemellus muscles
- autonomic ganglia and plexuses
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta previa
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumors
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumors of the testis
- testicular seminoma
-
non seminomatous germ cell tumors
- mixed germ cell tumor
- yolk sac tumor (endodermal sinus tumor)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumor
- sex cord / stromal tumors of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumor of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumors (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumors
- ureteral trauma
- other
- bladder
- kidneys





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.