Nuchal translucency is the normal fluid-filled subcutaneous space identified at the back of the fetal neck during the late first trimester and early second trimester (11 weeks 3 days to 13 weeks 6 days).
It should not be confused with the nuchal fold, which is seen in the second trimester.
On this page:
Pathology
Increased nuchal translucency is thought to be related to dilated lymphatic channels and is considered a nonspecific sign of more generalized fetal abnormality. Measurement of the nuchal translucency requires specific and standardized assessment and careful attention to technique.
Associations
Thickening of the nuchal translucency can be associated with a number of anomalies, including:
-
trisomies (including Down syndrome)
-
non-aneuploidy structural defects and syndromes
congenital heart disease: risk varies from 2% at the 95th percentile to 5% at the 99th percentile (3.5 mm), with septal defects the commonest abnormality 10
Noonan syndrome: the only genetic molecular condition with a clear association with increased nuchal translucency
miscarriage or fetal demise: the risk is directly proportionate to increased nuchal translucency thickness and ranges from 1.6% with NT between 95-99th percentile to 20% with NT >6.5 mm 11
intrauterine infections: parvovirus B19 is the only specific pathogen with direct relation to increased NT due to the effect of fetal anemia and fetal myocardial infarction
Radiographic features
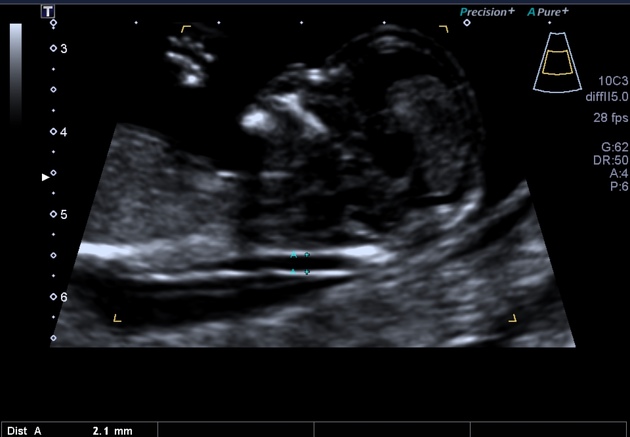
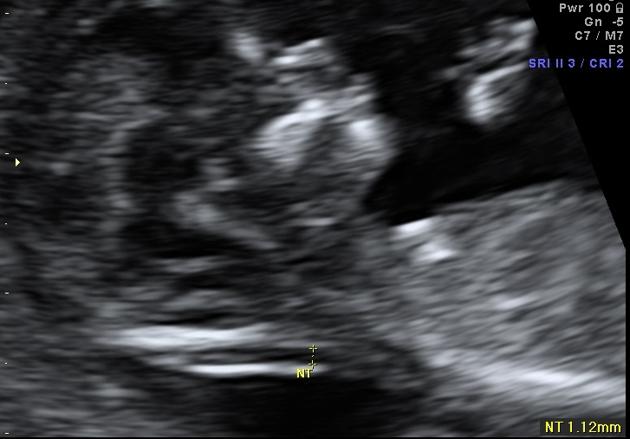
Nuchal lucency is measured on a sagittal image through the fetal neck.
Technique
Use of the correct technique is essential 15:
-
the fetus must be in the midsagittal imaging plane (the vertebral column should be facing the bottom of the screen); the following structures must be seen to confirm the correct mid-sagittal position:
-
two tiny parallel echogenic lines
tip of the nose
nasal bone (if not absent)
diencephalon
-
magnification so that only the fetal head and upper thorax are included in the image: allowing for 0.1 mm changes in measurement.
the fetal head should not be extended or flexed
the fetus should be floating free of the uterine wall i.e. amniotic fluid should be seen between its back and the uterus; this is to not mistakenly measure the distance to the amniotic membrane or uterine wall
-
the "+" calipers should be used for measurement
only the lucency is measured (again differing from nuchal thickness)
the calipers are placed inside the hyperechoic edges
the widest part of the translucency should be measured
Assessment
values obtained when the CRL is between 45 and 84 mm (11 weeks 3 days to 13 weeks 6 days) may be used for combined first-trimester screening
the lucent region is generally not septated
the thickness rather than the appearance (morphology) is considered to be directly related to the incidence of chromosomal and other anomalies
a value of less than 2.2-2.8 mm in thickness is not associated with increased risk, however, it is maternal age-dependent and needs to be matched to exact gestational age and crown-rump length (CRL)
Nuchal translucency cannot be adequately assessed if there is:
unfavorable fetal lie
unfavorable gestational age: CRL <45 or >84 mm
Interpretation
Increased NT is considered when it measures >95th percentile for a given crown rump length (CRL) 14. The rate of aneuploidy is directly proportional to the value of nuchal translucency 9:
<2 mm have a risk of <1%.
3.4 mm have a risk of 7%
3.5-4.4 mm have a risk of 20%
5.5-6.4 mm have a risk of 50%
≥8.5 mm have a risk of 75%
In the majority of fetuses with trisomy 21, the nuchal translucency thickness was <4.5 mm, while with trisomies 13 or 18 it was 4.5-8.4 mm, and in those with Turner syndrome, it was 8.5 mm or more 9.
Correlation with serum markers
To increase the clinical accuracy of nuchal lucency, it can be correlated with serum markers such as:
estriol/estriol
The combination of nuchal translucency thickness, PAPP-A, and hCG detects 87% of cases of trisomy 21 at 11 weeks, 85% at 12 weeks, and 82% at 13 weeks, with a 5% false-positive rate 8.
Further workup
If abnormal NT and screening test results show an increased risk of less than 1 in 300, further workup may be carried out based on the patient's desire after counseling. Further investigations include:
Treatment and prognosis
As the second-trimester approaches, the region of nuchal translucency might either:
-
regress
if chromosomally normal, a large proportion of fetuses will have a normal outcome
spontaneous regression does not, however, mean a normal karyotype
-
evolve into
-
normal outcome: the change is proportionate to NT value 12
3.5-4.4 mm have a chance of 70%
4.5-5.4 mm have a chance of 50%
5.5-6.4 mm have a chance of 30%
>6 mm have a chance of 15%
History and etymology
The Terminologia Anatomica refers to the neck as a whole as the "collum". In official Latin anatomical nomenclature, "cervix" refers to the front of the neck and "nucha" to the back (nape) of the neck 13.
Differential diagnosis
incorrect technique
fetal neck skin thickening due to first-trimester hydrops fetalis
amniotic membrane lying behind the fetal neck
External links
If any of these links are broken or for other problems and questions, please contact editors@radiopaedia.org.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.