Prostate cancer ranks as the most common primary malignant tumor in men and the second most common cause of cancer-related deaths in men. Prostatic adenocarcinoma is by far the most common histological type and is the primary focus of this article.
On this page:
Terminology
The aim of prostate MRI is to detect clinically significant prostate cancer, as insignificant prostate cancer is common 35. However, this term is without a consensus definition 35,36 (c. 2024) and has been defined as one or more of the following (noting variability within criterion) 31-35:
prostate-specific antigen (PSA) >10 ng/mL or PSA density >0.15 ng/mL
tumor volume >0.5 mL (translates to a focus of ≥8 x 8 x 8 mm)
extraprostatic extension (on biopsy or imaging)
-
Gleason score >6 or ≥7
maximum number of positive biopsy samples >2
tumor volume within the biopsy sample >50%
ISUP grade group 2 or 3, or higher
NB variables related to biopsy results will obviously not be available in primary detection cases.
Epidemiology
It is primarily a disease of the elderly male. In the United States, approximately 200,000 new cases are diagnosed each year.
Clinical presentation
Prostate cancer is usually detected by:
an elevated (greater than 4 ng/dL) prostate-specific antigen (PSA); normal is 1-4 ng/dL
-
abnormal digital rectal examination
the prostate gland is divided into several anatomic zones and prostate cancer usually arises within the peripheral zone near the rectum, which is why a digital rectal exam (DRE) is a useful screening test
Clinically patients can present with:
-
urinary symptoms, e.g. nocturia, hesitancy, urgency, terminal dribble
often collectively known as LUTS (lower urinary tract symptoms)
hematuria (in advanced disease) 27
back pain (from metastatic spread to the spine)
Clinical scores that may be useful in assessing symptoms severity include:
IPSS: international prostate symptoms score, 35 points score mainly assessing urinary symptoms
Pathology
95% of prostate cancers are adenocarcinomas that develop from the acini of the prostatic ducts 15. They arise in the posterior/peripheral (70%) prostate gland more commonly than in the anterior gland and central zone (30%) 21.
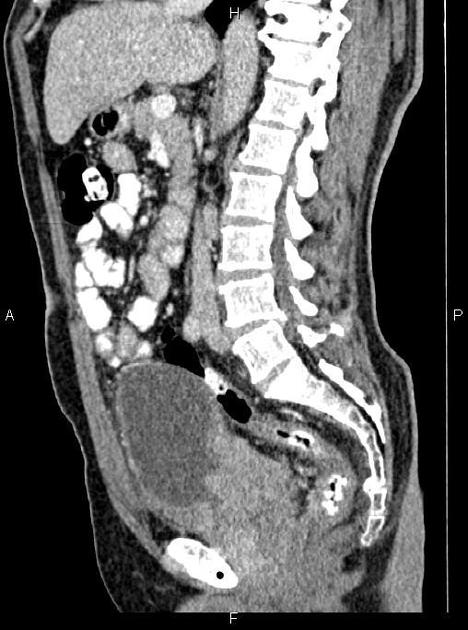
Prostate cancer can spread by local invasion (typically into the bladder and seminal vesicles; urethral and rectal involvement are rare), lymphatic spread (pelvic nodes first followed by para-aortic and inguinal nodes), or by hematogenous metastases 23. Common sites of hematogenous metastases are 22,23:
bone (90%)
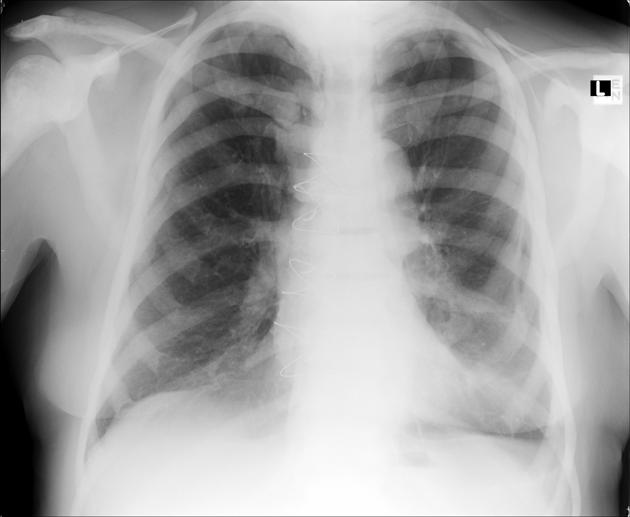
lung (~45%)
liver (~25%)
pleura (~20%)
adrenal glands (~15%)
Microscopic appearance
Pathologic specimens are graded using the Gleason score, which is the sum of the most prevalent and second most prevalent types of dysplasia, each on a scale of 1 to 5, with 5 being the most dysplastic.
Staging
The TNM staging system is used for staging prostate cancer. Prostate cancer is one of the (less common) causes of cannonball metastases to the lung.
Genetics
The probability of developing prostate cancer seems to depend on the presence of five polymorphisms (SNPs) in the genome 28.
Radiographic features
Ultrasound
Transrectal ultrasonography (TRUS) is often initially performed to detect abnormalities and to guide biopsy, usually following an abnormal PSA level or DRE.
Ultrasound is used to direct the biopsy of suspicious, hypoechoic regions, usually in the peripheral zone. Because of the high incidence of multifocality, systematic sextant biopsies are recommended.
On ultrasound, prostate cancer is usually seen as a hypoechoic lesion (60-70%) in the peripheral zone of the gland but can be hyperechoic or isoechoic (30-40% of lesions).
Transrectal ultrasound is also the modality of choice for directing brachytherapy seeds into the prostate gland.
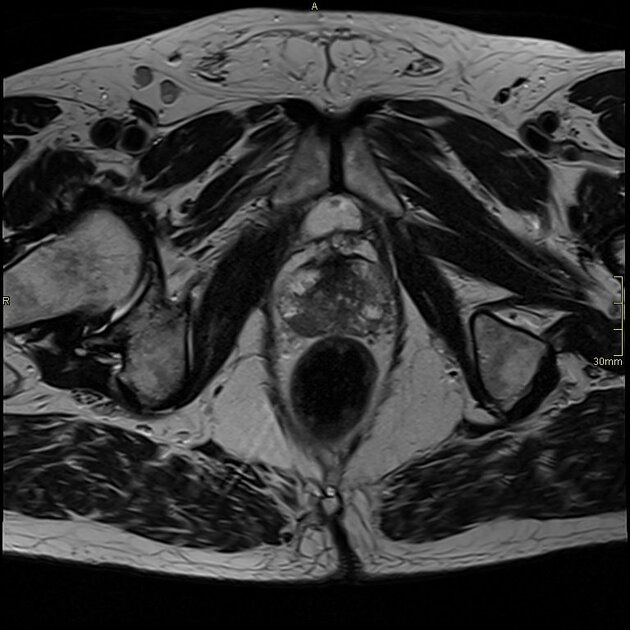
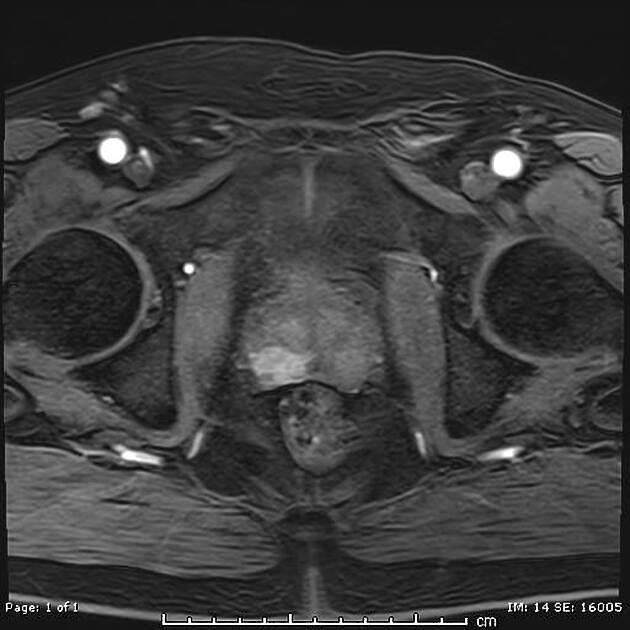
MRI
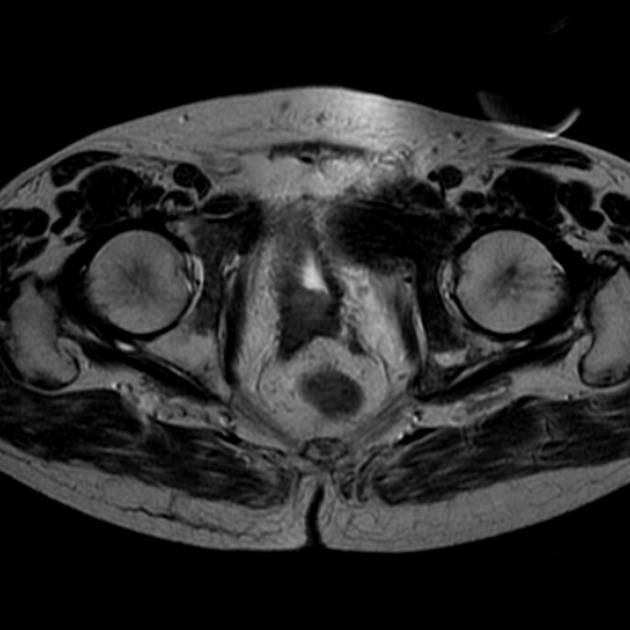
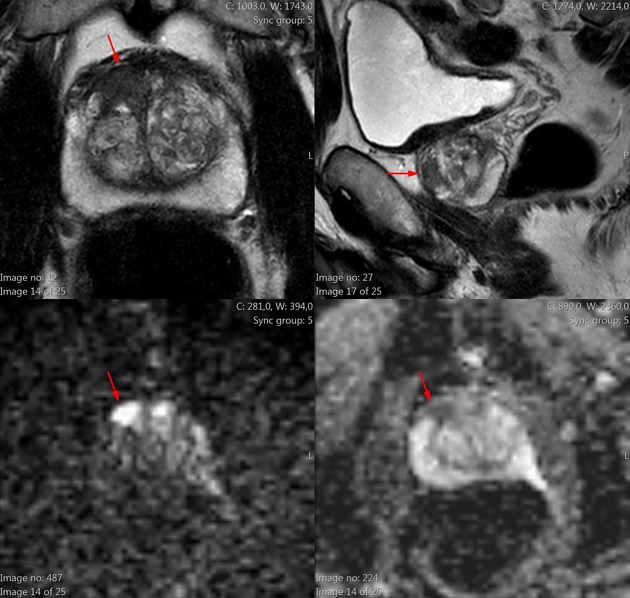
The primary indication for MRI of the prostate is in the evaluation of prostate cancer after an ultrasound-guided prostate biopsy has confirmed cancer in order to determine if there is extracapsular extension 1,2,4. Increasingly MRI is also being used to detect and localize cancer when the PSA is persistently elevated, but routine TRUS biopsy is negative. Both the American College of Radiology (ACR) and the European Society of Uroradiology (ESUR) advocate the use of multiparametric MRI (mpMRI) in prostate imaging 20.
MRI-guided prostate biopsy is also being used, particularly in those cases where TRUS biopsy is negative but clinical and PSA suspicion remains high 12. Following radical prostatectomy, patients with elevated PSA should also be examined using MRI.
Often a PI-RADS score is given to assess the probability of the lesion being malignant.
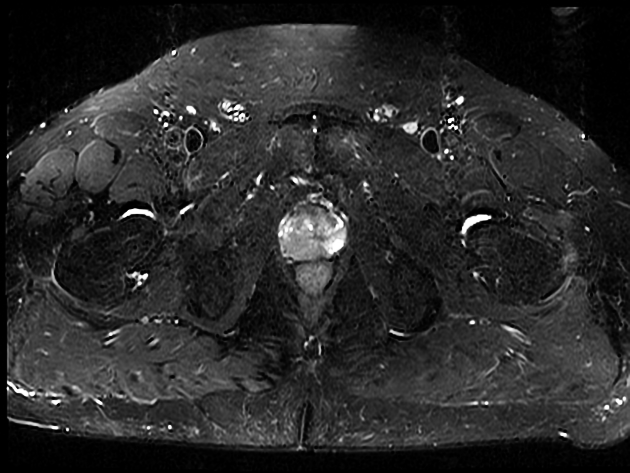
Signal characteristics
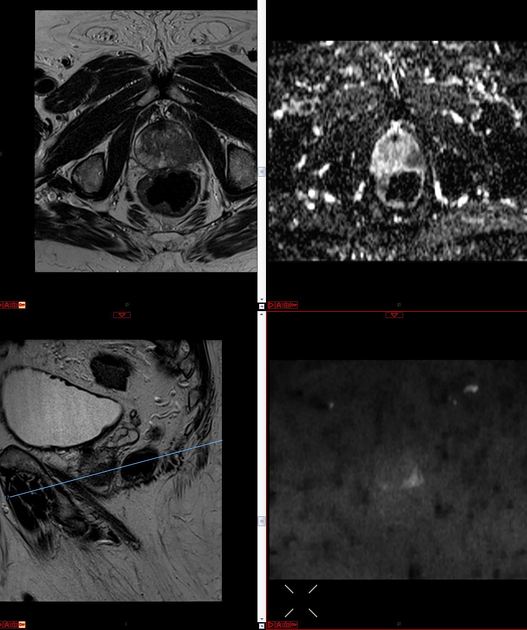
T1: useful for detection of prostate contour, neurovascular bundle encasement, and post-biopsy hemorrhage 15
-
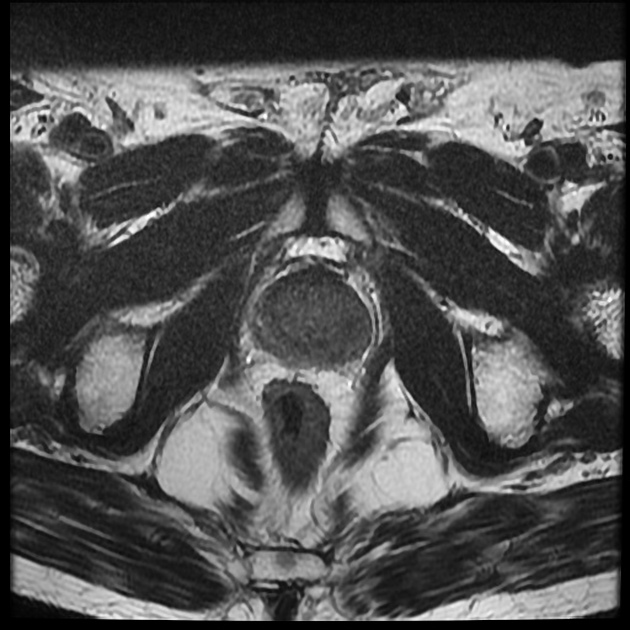
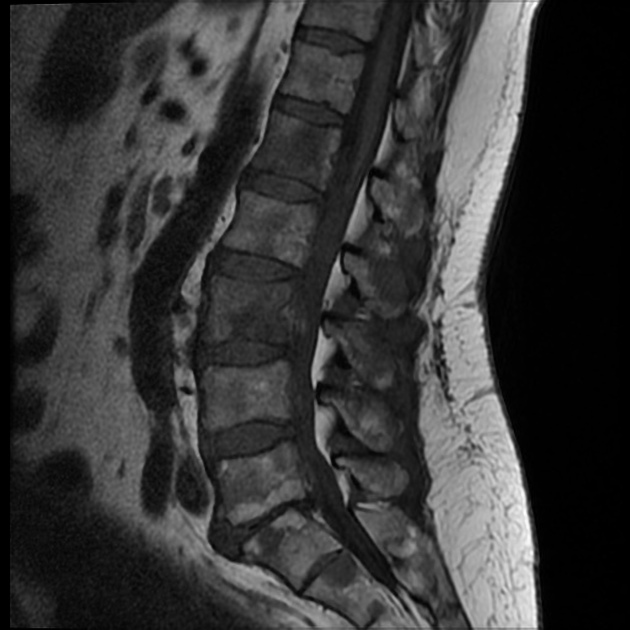
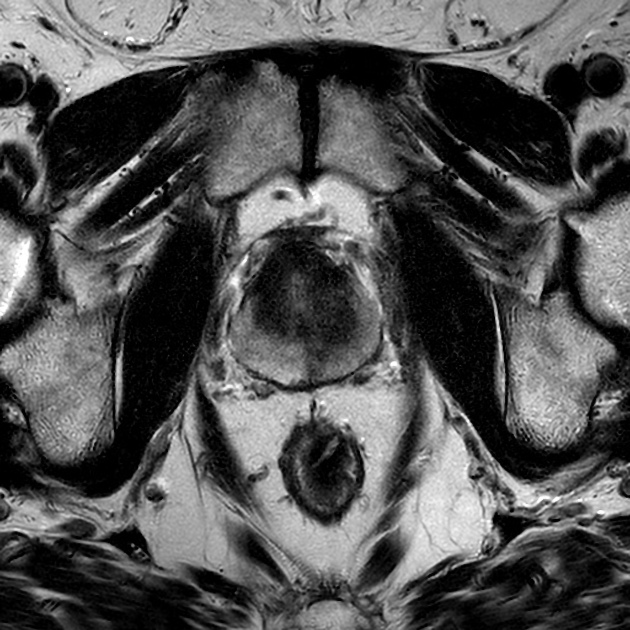
T2
using an endorectal coil, on T2-weighted images prostate cancer usually appears as a region of low signal within a normally high signal peripheral zone 1,13
most significant cancers occur along the posterior portion of the prostate gland abutting the rectum
DWI/ADC: often shows restricted diffusion
-
dynamic contrast enhancement (DCE): (dynamic contrast enhancement in prostate cancer)
shows enhancement but it can be difficult to distinguish from prostatitis or benign prostatic hyperplasia (especially in the central zone lesions 19)
more specific than T2 signal 17
involves post-processing time
-
MR spectroscopy: (MR-spectroscopy in prostate cancer)
increased choline: citrate or choline+creatine: citrate ratios are seen in prostate cancer (see below for more details) 15
Routine use of body 3.0 T magnets now means that endorectal coils have become unnecessary for prostate imaging due to the improved signal to noise and spatial resolution associated with higher field strength.
MRI parameters routinely assessed include the presence of a mass with a low T2 signal, restricted diffusion with reduced ADC, and increased tissue capillary permeability using dynamic contrast-enhanced (DCE) imaging and calculation of the so-called Ktrans (a calculated time constant for permeability). These so-called multiparametric techniques are increasingly being used in the assessment of prostate malignancy with MRI 11.
Extracapsular extension carries a poor prognosis. Assess for:
asymmetry/extension into the neurovascular bundles
obliteration of the rectoprostatic angle
involvement of the urethra
seminal vesicle invasion (normal seminal vesicles have a high signal on T2)
Lymphadenopathy is best appreciated on T1-weighted images.
MR spectroscopy
The addition of MR spectroscopy (MRS) with fast T2-weighted imaging is an area of research that holds promise for the detection of disease. The normal prostate produces a large amount of citrate from the peripheral zone, which tumors do not 3. In normal prostate tissue citrate and polyamine levels are high and choline levels low. The reverse is the case in a tumor.
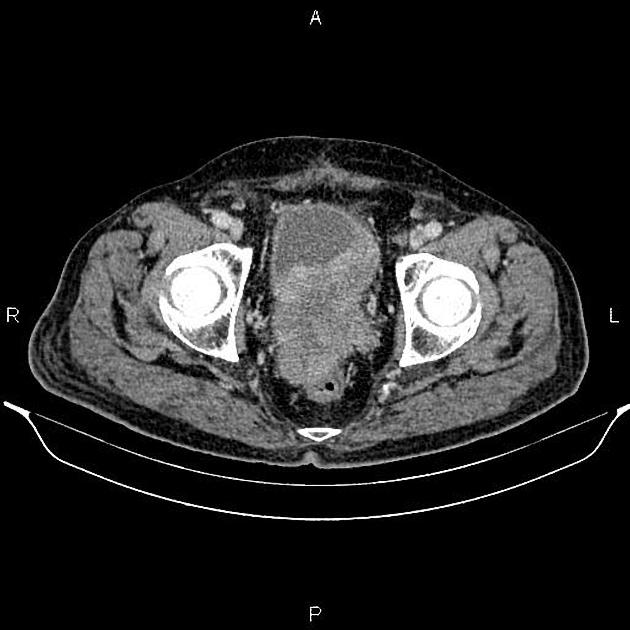
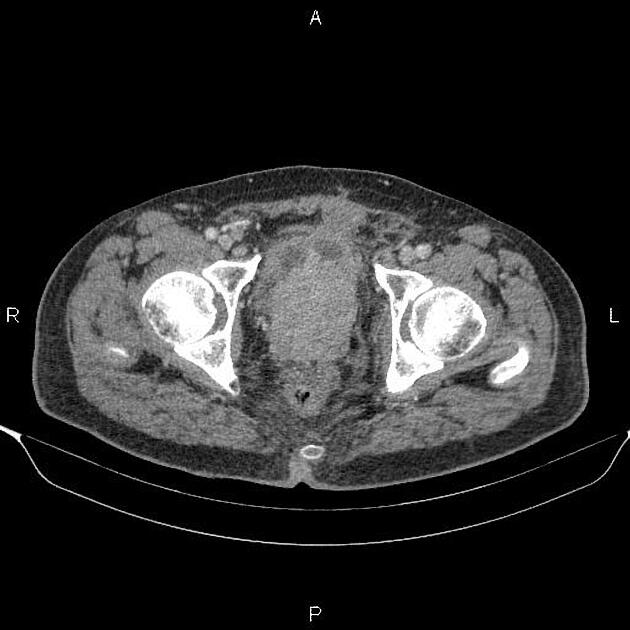
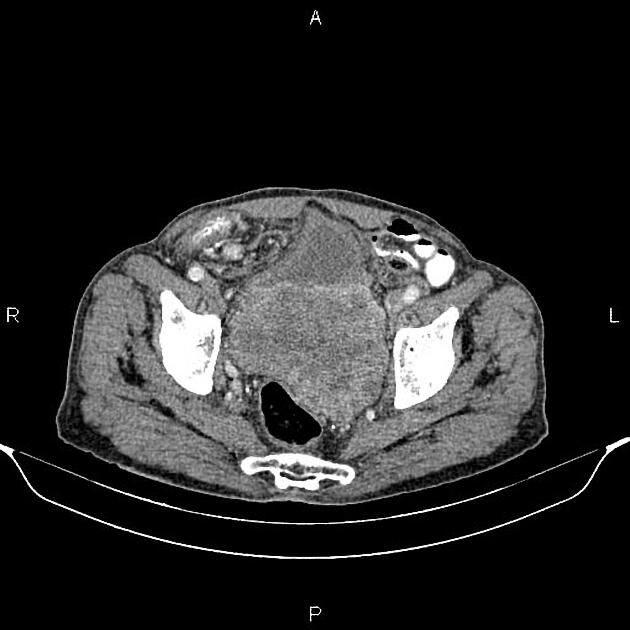
CT
Not accurate at detecting in situ prostate cancer. Scans of the abdomen and pelvis are commonly obtained before the onset of radiation therapy to identify bony landmarks for planning.
In advanced disease, a CT scan is the test of choice to detect enlarged pelvic and retroperitoneal lymph nodes, hydronephrosis, and osteoblastic metastases 5.
Nuclear medicine
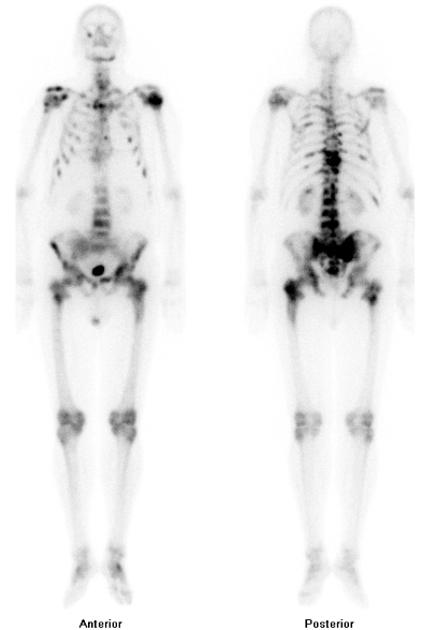
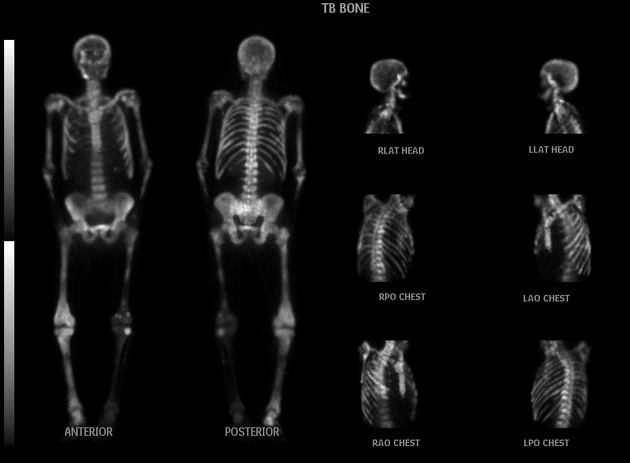
Tc-99m MDP bone scan
technetium-99m bone scan is usually used to detect osseous metastases
Ga-68-PSMA PET
gallium-68-PSMA PET can be used for diagnosis, staging, restaging, evaluation of therapy response and prognostication in prostate cancer 26
F-18 PSMA PET
fluorine-18-PSMA PET can also be used for diagnosis, staging, restaging and evaluation of therapy response. Fluorinated tracers have a longer half-life and are therefore more practical than gallium tracers.
in patients with low PSA levels, F-18 PSMA PET or Ga-68 PSMA PET is superior in detecting prostate cancer metastases compared to PET performed with other radiotracers 29
F-18-fluciclovine PET
fluorine-18-fluciclovine PET is used to detect and localize suspected prostate cancer recurrence based on elevated prostate-specific antigen in men who have undergone prior treatment
F-18 FDG PET
FDG PET may be used for PSMA negative patients with aggressive cancer or to assess recurrence 30
Treatment and prognosis
Generally, patients with a Gleason score of <7 and a PSA of <10 ng/L are considered to have a potentially curable disease. These patients undergo prostatectomy, brachytherapy, or external beam radiation 5.
Patients that do not meet these criteria will usually undergo a combination of androgen deprivation therapy, immunotherapy, radiotherapy, or chemotherapy. Theranostic approaches including PSMA-targeted therapies e.g. lutetium-177 vipivotide tetraxetan, are increasingly emerging for prostate cancer management, particularly intractable metastatic disease.
Differential diagnosis
General imaging differential considerations include:
-
rhabdomyosarcoma of the prostate: different demographics 7, i.e. much younger age group
other prostatic tumors: rare (e.g. melanoma of prostate 9)
direct invasion of the prostate by bladder or rectal adenocarcinoma
Differential considerations (mimics) on MRI include 24:
anterior fibromuscular stroma: anterior, symmetric, usually hypointense
the central zone of the prostate: symmetric, central, tends not to wash out on DCE
periprostatic veins and periprostatic lymph nodes
amyloidosis (rare)
calcification, necrosis, hemorrhage

























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.