Ovarian mucinous cystadenoma
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
View Yuranga Weerakkody's current disclosuresAt the time the article was last revised Peter John Bandura had no recorded disclosures.
View Peter John Bandura's current disclosures- Mucinous cystadenoma of the ovary
- Mucinous cystadenoma of ovary
- Ovarian mucinous cystadenomas
- Mucinous cystadenomas of the ovary
- Mucinous cystadenomas of ovary
Mucinous cystadenoma of the ovary is at the benign end of the spectrum of mucin-containing epithelial ovarian tumors.
On this page:
Epidemiology
The estimated peak incidence is at around 30-50 years of age.
They comprise approximately 80% of mucinous ovarian tumors and 20-25% of all benign ovarian tumors.
Pathology
The tumors are lined by columnar epithelium, typically similar to endocervical epithelium, though occasionally an intestinal-type may be seen. These cells secrete thick, gelatinous mucin which fills the locules 5.
Radiographic features
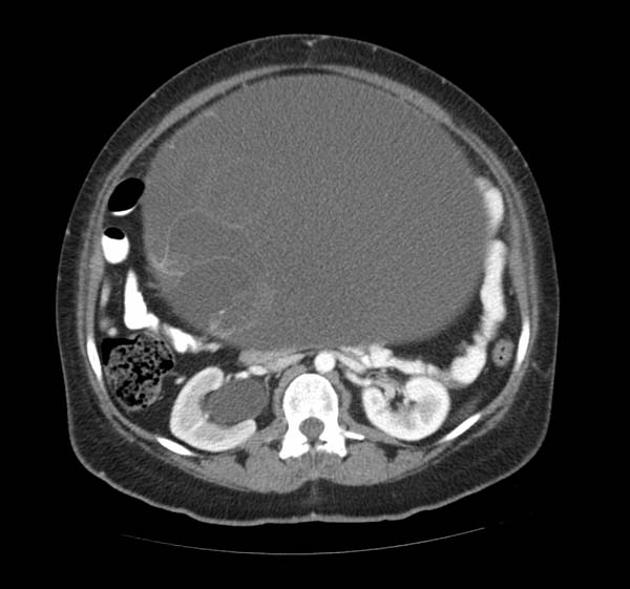
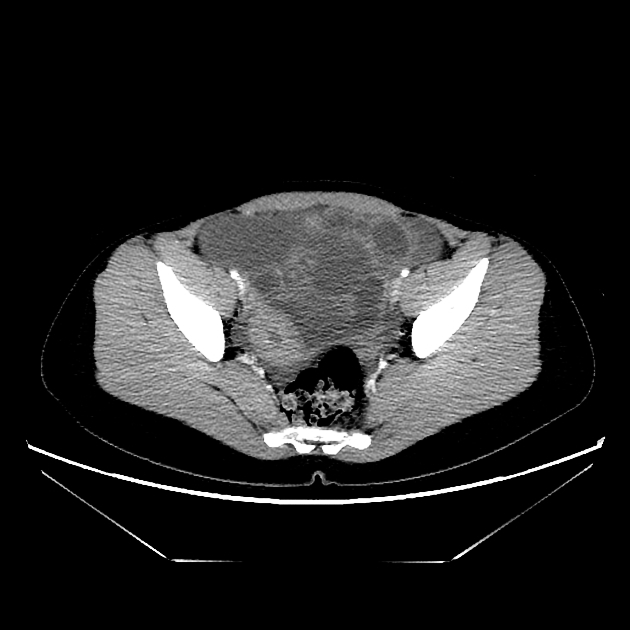
Mucinous cystadenomas tend to be larger than serous cystadenomas at presentation 1. Bilaterality is rare (2-5%). Mural calcification is more common than serous tumors 6.
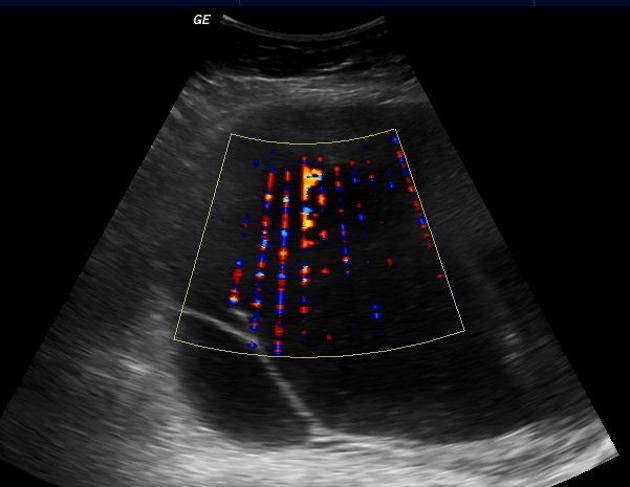
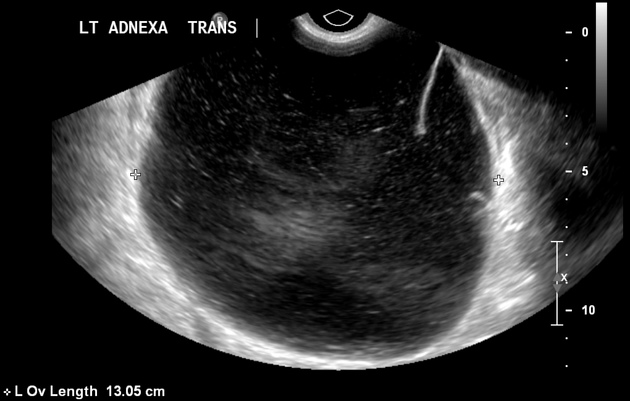
Ultrasound
- typically large cystic adnexal mass
- multilocular with numerous thin septations
- loculations may contain low-level internal echogenicity due to increased mucin content
- different locules may contain various degrees of echogenicity
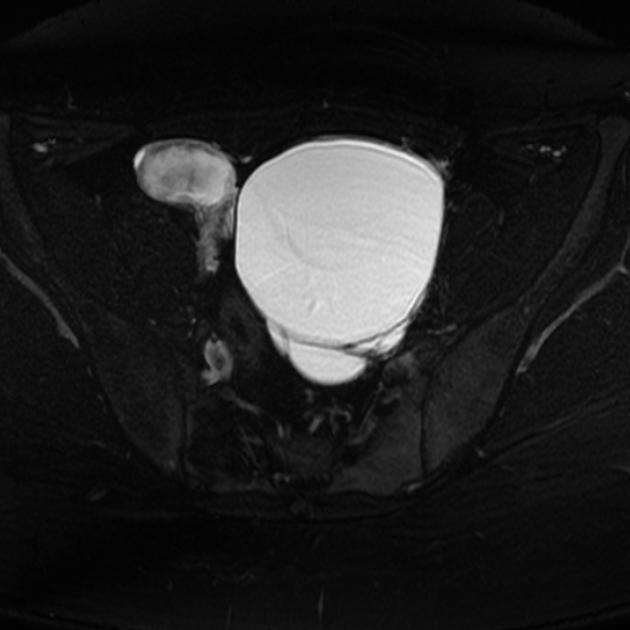
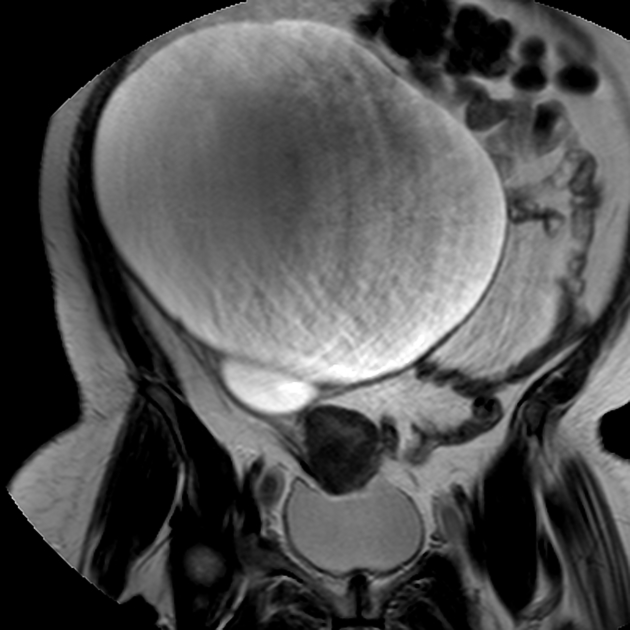
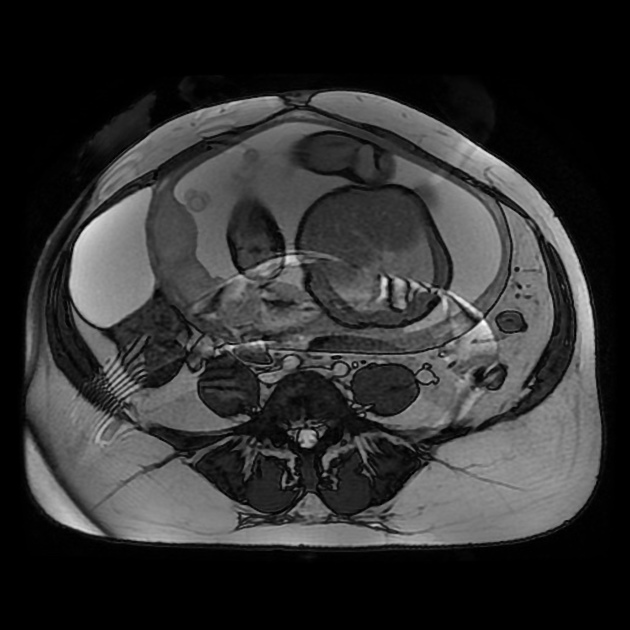
MRI
Mucinous cystadenomas are usually seen as large multilocular cysts containing fluid of various viscosity. Due to this reason, the loculi of the tumors often show variable signal intensities on both T1 and T2 sequences. This can sometimes give a “stained glass” appearance. They rarely appear as unilocular cysts.
Treatment and prognosis
A mucinous cystadenoma is benign with excellent prognosis (cf. borderline mucinous tumors of the ovary or mucinous cystadenocarcinoma of the ovary). Nonetheless, they are frequently surgically excised for histological confirmation of benignity, and due to mass effect of the large tumors.
See also
References
- 1. Jung SE, Lee JM, Rha SE et-al. CT and MR imaging of ovarian tumors with emphasis on differential diagnosis. Radiographics. 22 (6): 1305-25. doi:10.1148/rg.226025033 - Pubmed citation
- 2. Mullen CJ, Burd D, Reuter KL. Magnetic resonance imaging of an ovarian mucinous cystadenoma immediately before and after rupture. Br J Radiol. 1997;70 (834): 654-5. Br J Radiol (abstract) - Pubmed citation
- 3. Imaoka I, Wada A, Kaji Y et-al. Developing an MR imaging strategy for diagnosis of ovarian masses. Radiographics. 26 (5): 1431-48. doi:10.1148/rg.265045206 - Pubmed citation
- 4. Tanaka YO, Nishida M, Kurosaki Y et-al. Differential diagnosis of gynaecological "stained glass" tumours on MRI. Br J Radiol. 1999;72 (856): 414-20. Br J Radiol (abstract) - Pubmed citation
- 5. Crum CP (1999). The female genital tract. In Cotran RS, Kumar VK, and Collins T (Eds.), Robbins pathologic basis of disease (pp. 1035-1091). Philadelphia: Saunders
- 6. Okada S, Ohaki Y, Inoue K et-al. Calcifications in mucinous and serous cystic ovarian tumors. J Nippon Med Sch. 2005;72 (1): 29-33. Pubmed citation
- 7. Taylor EC, Irshaid L, Mathur M. Multimodality Imaging Approach to Ovarian Neoplasms with Pathologic Correlation. (2021) Radiographics : a review publication of the Radiological Society of North America, Inc. 41 (1): 289-315. doi:10.1148/rg.2021200086 - Pubmed
- 8. Marko J, Marko KI, Pachigolla SL, Crothers BA, Mattu R, Wolfman DJ. Mucinous Neoplasms of the Ovary: Radiologic-Pathologic Correlation. (2019) Radiographics : a review publication of the Radiological Society of North America, Inc. 39 (4): 982-997. doi:10.1148/rg.2019180221 - Pubmed
- 9. Brown J, Frumovitz M. Mucinous tumors of the ovary: current thoughts on diagnosis and management. (2014) Current oncology reports. 16 (6): 389. doi:10.1007/s11912-014-0389-x - Pubmed
Incoming Links
- Mucinous cystadenoma of the ovary
- Ovarian cystadenoma
- Ovarian collision tumour
- Ovarian mucinous cystadenoma
- Ovarian mucinous cystadenoma identified in pregnancy (MRI)
- Ovarian mucinous cystadenoma
- Mucinous cystadenoma of the ovary
- Cervical cancer and Brenner tumour (gross pathology)
- Benign seromucinous cystadenoma of the ovary
- Colon adenocarcinoma with Krukenberg tumors, advanced pregnancy
- Mucinous cystadenoma of the ovary
- Ovarian mucinous cystadenoma
- Ovarian mucinous cystadenoma and adenomyosis
- Borderline mucinous cystadenoma of ovary
- Ovarian mucinous cystadenoma
- Ovarian mucinous cystadenoma
- Ovarian mucinous cystadenoma
- Ovarian mucinous cystadenoma (gross pathology)
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta previa
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumors
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumors of the testis
- testicular seminoma
-
non seminomatous germ cell tumors
- mixed germ cell tumor
- yolk sac tumor (endodermal sinus tumor)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumor
- sex cord / stromal tumors of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumor of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumors (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumors
- ureteral trauma
- other
- bladder
- kidneys











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.