Endometrial carcinoma is generally considered the most common gynecological malignancy. It frequently presents with vaginal bleeding. Both ultrasound and pelvic MRI are useful modalities for evaluation.
On this page:
Epidemiology
Endometrial carcinoma is the most common gynecological malignancy, with peak incidence at around the 6th decade, though 12% of cases present in premenopausal women.
The overall incidence is thought to be increasing. In the United States, there is a greater incidence among patients of European descent compared to those of African-American descent.
Risk factors
The risk factors for endometrial carcinoma are anything that leads to increased estrogen exposure 21:
estrogen replacement therapy
polycystic ovarian syndrome and anovulatory cycles
tamoxifen
early menarche or late menopause
nulliparity
estrogen-producing ovarian tumors, e.g. granulosa cell cancer
Smoking may be protective 22.
Associations
hereditary non-polyposis colon cancer (HNPCC) 4: estimated 30-50x increased lifetime risk
precursor lesions of complex hyperplasia with atypia are associated with endometrial carcinoma in over 40% of cases 4
Clinical presentation
Patients commonly present at an early stage, with postmenopausal bleeding as the initial symptom (present in 90% of patients 17).
Pathology
Endometrial carcinoma is divided into two subtypes - type I and type II. The majority are adenocarcinoma.
Type I endometrial carcinoma
Type I (80%) arises in the setting of unopposed hyperestrogenism and endometrial hyperplasia. It is mostly seen in obese women between 55 to 65 years old and is a well-differentiated tumor with relatively slow progression and a more favorable outcome 19. PTEN gene mutation occurs in 30-80% of cases.
Type II endometrial carcinoma
Type II (20%) arises in the setting of endometrial atrophy, in females between 65 to 75 years old, and endometrial intraepithelial carcinoma. p53 mutation occurs in up to 50%. This type tends to be less differentiated and spread early via lymphatics or through fallopian tubes into the peritoneum, hence it is associated with a poorer prognosis compared to type I lesions.
Histology
Histological subtypes include:
-
type I
endometrioid carcinoma of the endometrium: commonest histological type: ~85%
-
type II
Other rare types
endometrial carcinoma with yolk sac tumor-like differentiation 24
Staging
Most tumors (~80%) present as stage I disease. Endometrial cancer is one of the (less common) causes of cannonball metastases to the lung. See endometrial carcinoma staging for further information.
Radiographic features
Transvaginal ultrasound is the initial imaging investigation of choice for patients presenting with the usual symptom of a postmenopausal bleed. A thickened endometrium requires endometrial sampling.
Staging of endometrial carcinoma is based on the FIGO staging system, which is a surgical and pathological staging following total abdominal hysterectomy, salpingo-oophorectomy, lymphadenectomy, and peritoneal washings. Such radical surgery may not be suitable for elderly patients or those with co-morbidities. MRI has a role in these patients in determining tumor extent and suitable therapy.
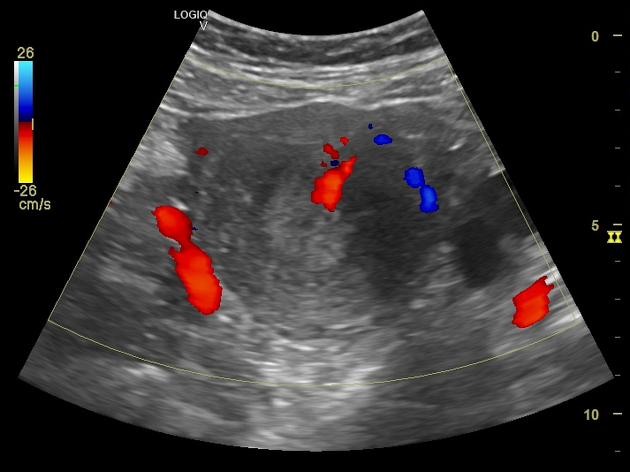
Ultrasound
Endometrial carcinoma usually appears as thickening of the endometrium though may appear as a polypoid mass.
-
premenopausal: normal endometrial thickness varies through the menstrual cycle
diagnosing abnormally thickened endometrium depends on knowing the patient's point in the menstrual cycle
postmenopausal: >5 mm is thickened (>8 mm if on hormone replacement therapy or tamoxifen) 17
Sonographic features are non-specific and endometrial thickening can also be due to benign proliferation, endometrial hyperplasia, or polyps. Ultrasound features that are suggestive of endometrial carcinoma rather than hyperplasia include 17:
heterogeneous and irregular endometrial thickening
polypoid mass lesion
intrauterine fluid collection
frank myometrial invasion
Disruption of a subendometrial halo on ultrasound may be suggestive of myometrial involvement.
In cases where transvaginal ultrasound is insufficient for endometrial evaluation, sonohysterography may be performed. During sonohysterography, the uterus is distended with sterile saline prior to ultrasound imaging, thus enabling full sonographic assessment of the endometrium with the transducer probe 23.
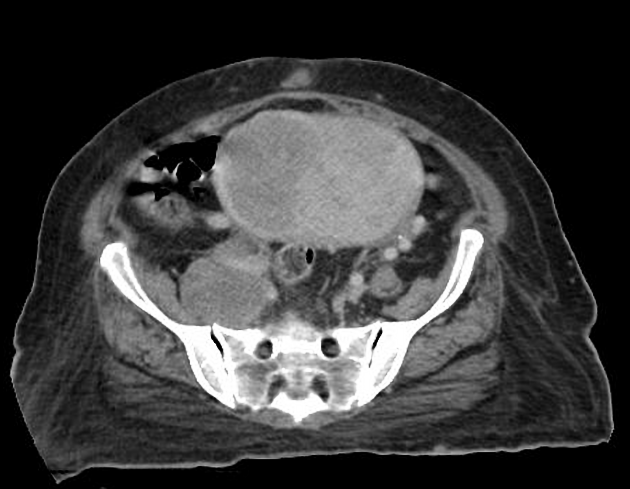
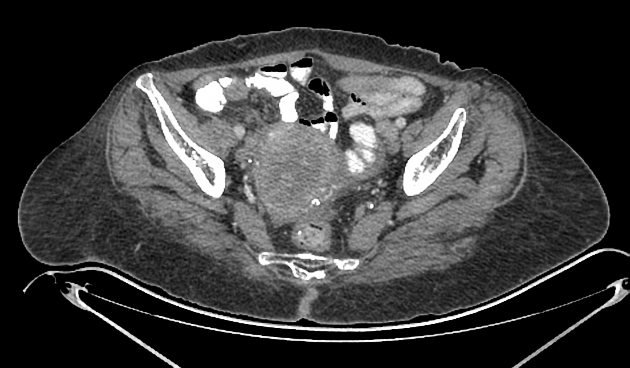
CT
CT has a role in assessing for distant metastases.
Although not generally used for initial diagnosis or local staging, endometrial carcinoma may be encountered on CT:
non-contrast CT: difficult to differentiate from the normal uterus (especially in local disease)
-
post-contrast CT
may show diffuse thickening or mass within the endometrial cavity
can also have an appearance of a hypoenhancing and hypoattenuating mass within endometrial cavity 18
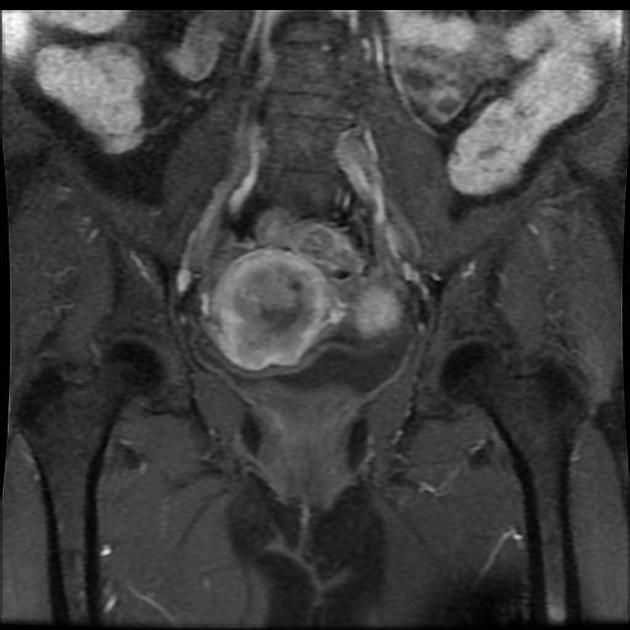
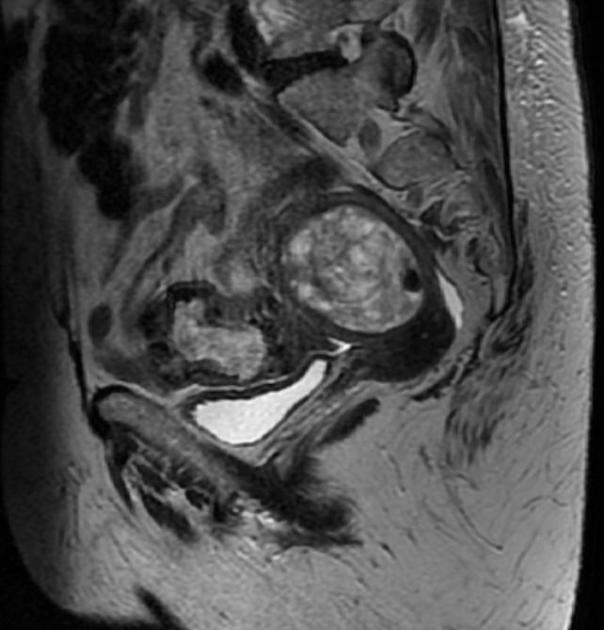
MRI
A dedicated pelvic MRI protocol is recommended for optimal disease extension assessment and is considered superior to CT for local staging 1,6. Contrast-enhanced MRI imaging improves accuracy in detecting myometrial invasion.
T1: hypo- to isointense to normal endometrium
-
T1 C+ (Gd)
carcinomatous tissue will enhance less than normal endometrium
dynamic contrast-enhanced sequences assist with assessment of the depth of myometrial invasion and delayed-phase images cervical stromal invasion ref
T2: iso to hypointense relative to normal endometrium, often heterogeneous; mildly hyperintense to myometrium, which forms the basis for assessment of myometrial invasion
DWI: impeded diffusion, also aids to assess the depth of myometrial invasion ref
FIGO stage
-
stage 1: tumor confined to the uterus
stage 1a: an invasion of less than half of the myometrium
stage 1b: an invasion of the outer half of myometrium
stage 2: tumor extends to the cervical stroma
-
stage 3: tumor extends beyond the uterus
stage 3a: tumor invades the serosa or adnexa
stage 3b: tumor invades the vagina or parametrium
-
stage 3c: pelvic/para-aortic lymph node involvement
3c1: pelvic lymph node involvement
3c2: para-aortic lymph node involvement
-
stage 4: bladder/rectal invasion or distant metastases
stage 4a: tumor extends into adjacent bladder or bowel
stage 4b: distant metastases
See the FIGO staging of endometrial cancer.
Nuclear medicine
PET-CT is inferior to MRI and ultrasound in the assessment of primary tumors, especially when small or in premenstrual women where there is normally increased physiological endometrial uptake 16.
Treatment and prognosis
Treatment usually involves a combination of surgery (mostly hysterectomy +/- bilateral salpingo-oophorectomy), chemotherapy and radiotherapy depending stage of the disease and patient factors. Hormone therapies may be employed for extra-uterine disease.
Prognosis depends on various factors including:
stage: depth of myometrial invasion, lymphovascular invasion, and nodal status
histological grade
Differential diagnosis
In early disease, the differential is essentially that of endometrial thickening:
submucosal uterine leiomyoma
Differential considerations for advanced lesions include:
-
carcinosarcoma of the uterus (previously known as malignant mixed Mullerian tumor (MMMT) of the uterus)
uterine lymphoma: rare (primary or secondary)
cervical cancer with uterine invasion
metastasis to the uterus from a non-gynecological malignancy: rare
Practical points
endometrial hyperplasia is a histologic diagnosis, it cannot be differentiated from early-stage endometrial carcinoma
-
postmenopausal vaginal bleeding is an important clinical sign for risk stratification of imaging findings
if present: endometrium >5 mm has 96% sensitivity in the detection of endometrial carcinoma
if not present: endometrium of >11 mm has been proposed as a threshold for endometrial biopsy 14









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.