Ovarian serous cystadenocarcinoma is the malignant form of ovarian serous tumor, the most common type of ovarian epithelial tumor. It is the most common type of ovarian malignancy.
Increasingly, high-grade serous carcinoma and low-grade serous carcinoma are recognized as distinct tumor types rather than a spectrum of disease grade as implied by the nomenclature (see Pathology for more).
On this page:
Terminology
Serous ovarian tumors are traditionally described with a "cyst-" prefix because of their primarily cystic composition, e.g. cystadenoma, cystadenocarcinoma.
Epidemiology
Account for the largest proportion of malignant ovarian tumors 1, representing over 50-80% of all malignant epithelial ovarian tumors 4. Serous ovarian cystadenocarcinomas account for ~25% of serous tumors.
The incidence peaks around the 6th to 7th decades of life 2.
Pathology
Macroscopic appearance
- multilocular cystic ovarian tumor with papillary projections
Microscopic appearance
- classified as high-grade versus low-grade carcinoma 9:
- high-grade serous carcinoma (HGSC)
- common (70-80%)
- thought to originate from distal fallopian tube epithelium
- high grade nuclear features (e.g. nuclear pleomorphism, abnormal mitotic figures)
- characterized by intratumoral heterogeneity
- nearly ubiquitous p53 positivity
- low-grade serous carcinoma (LGSC)
- uncommon (~5%) 9
- thought to mostly represent malignant degeneration of serous cystadenoma 9
- high-grade serous carcinoma (HGSC)
- psammoma bodies may be present in either low-grade serous carcinoma or high-grade serous carcinoma, but are more numerous in low-grade serous carcinoma 9
Risk factors
Recognized risk factors include:
- nulliparity
- early menarche
- late menopause
- positive family history
- infertility
Markers
- elevated serum CA-125 (>90% of cases 6)
Staging
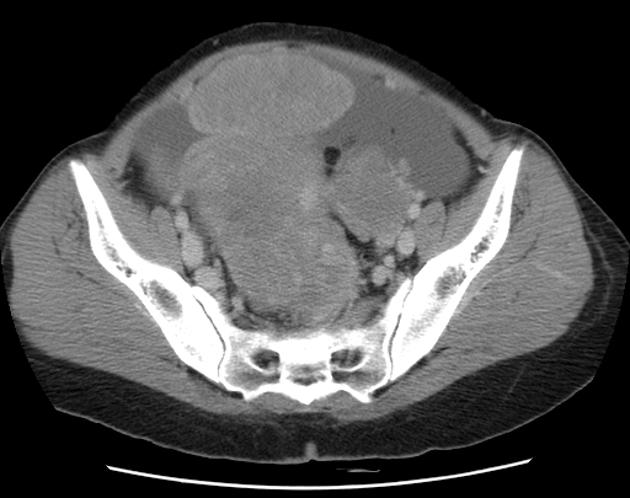
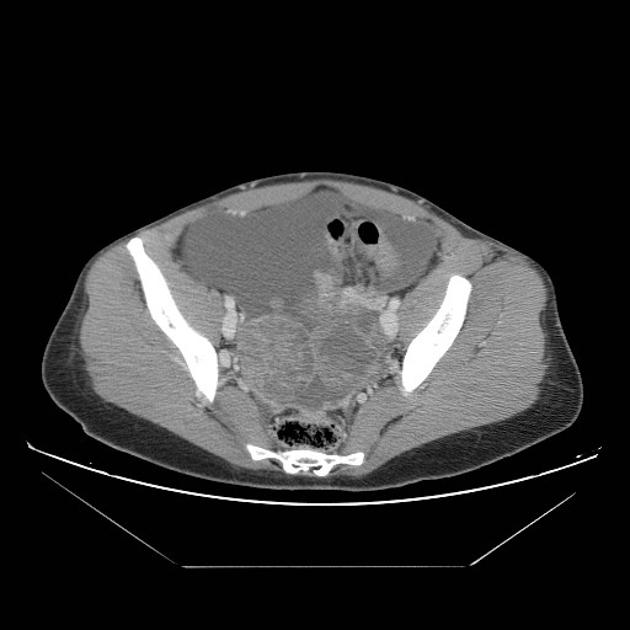
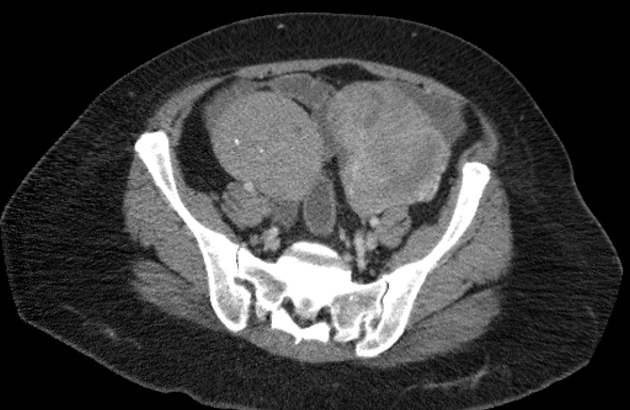
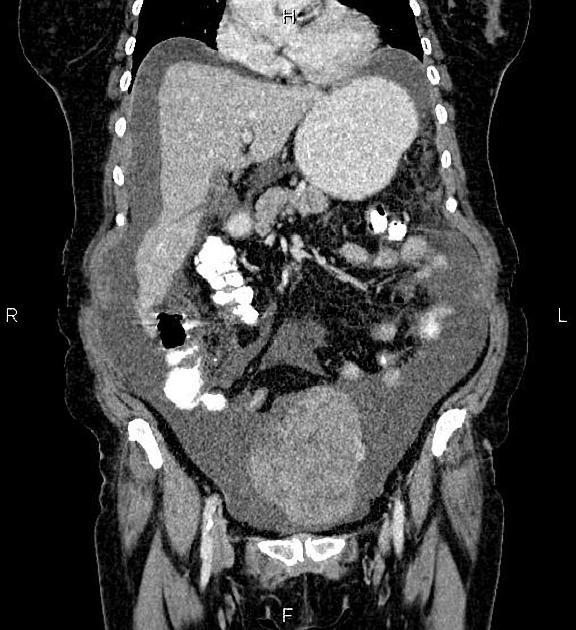
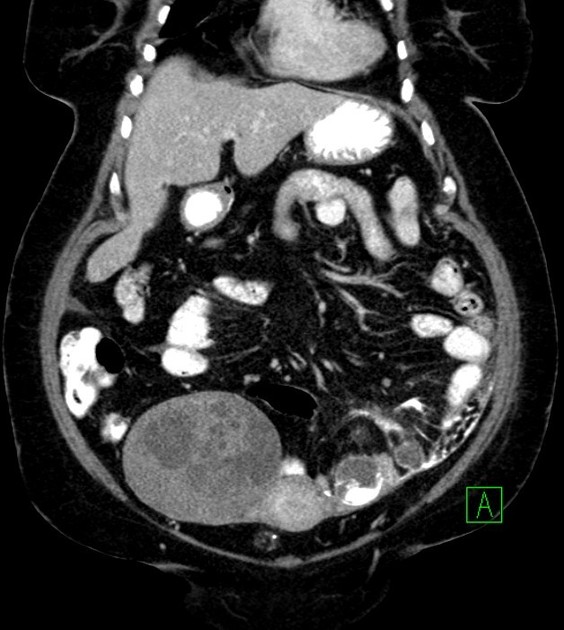
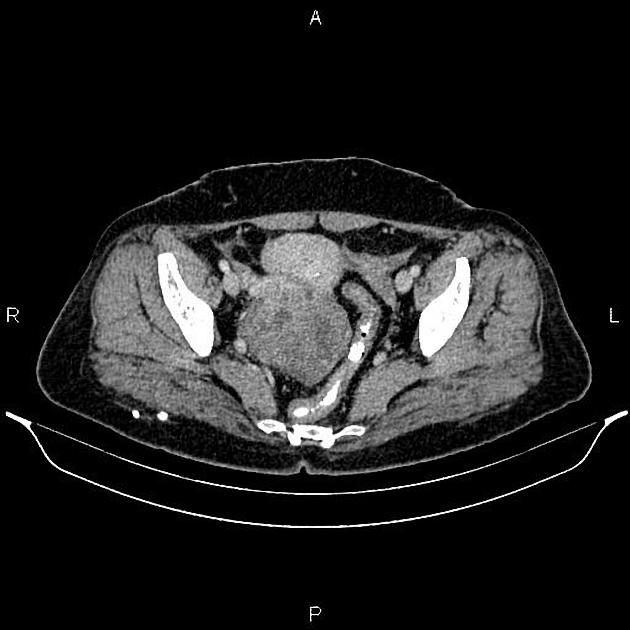
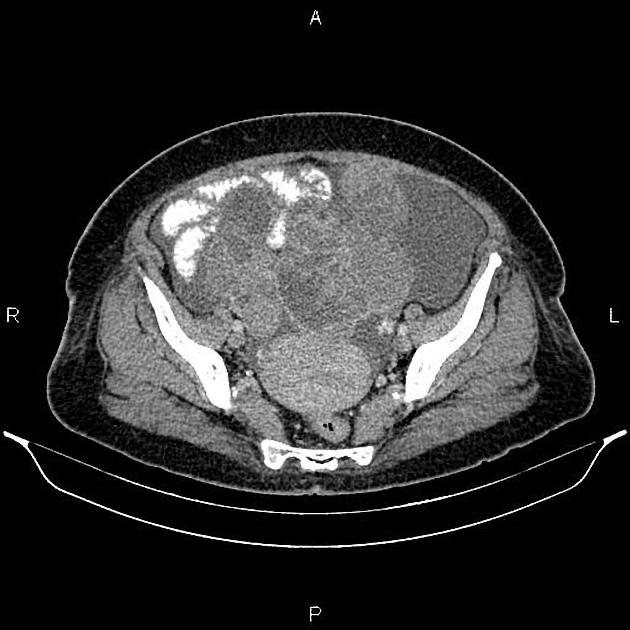
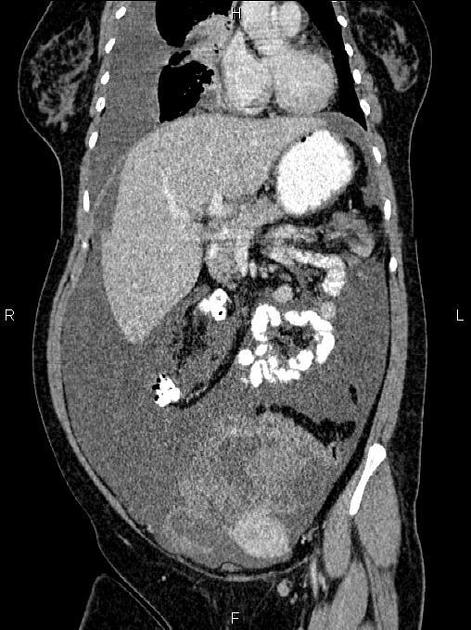
Radiographic features
Imaging plays an important role in the diagnosis of ovarian tumors and in the assessment for metastatic disease. However, surgical evaluation is the standard of care for the staging of disease.
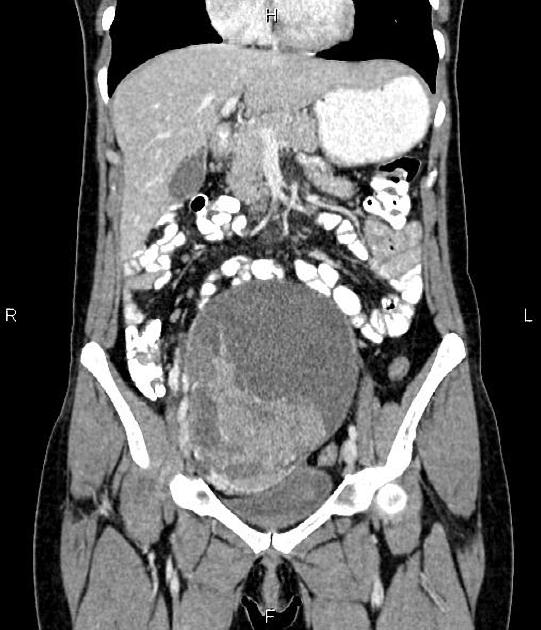
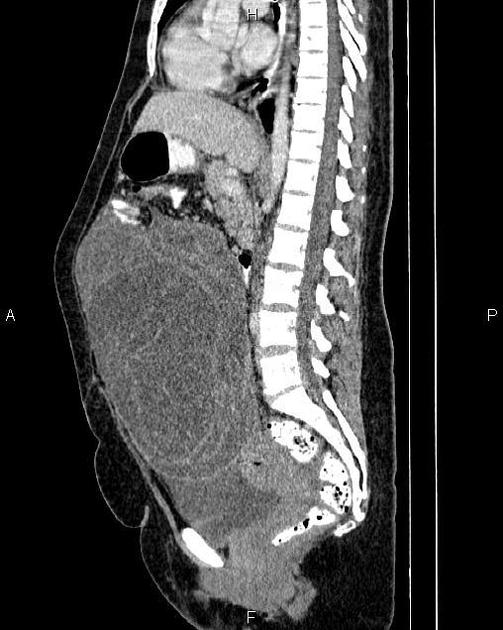
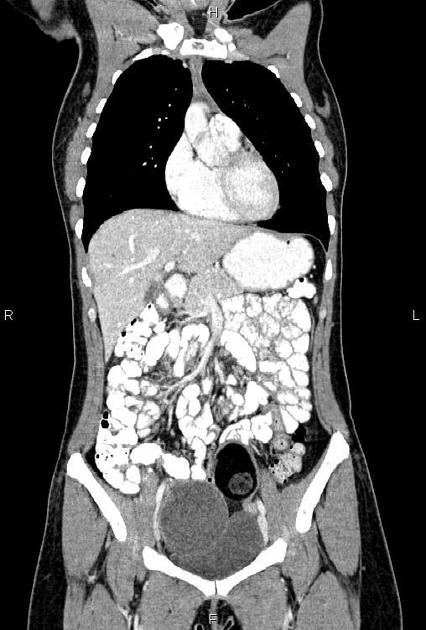
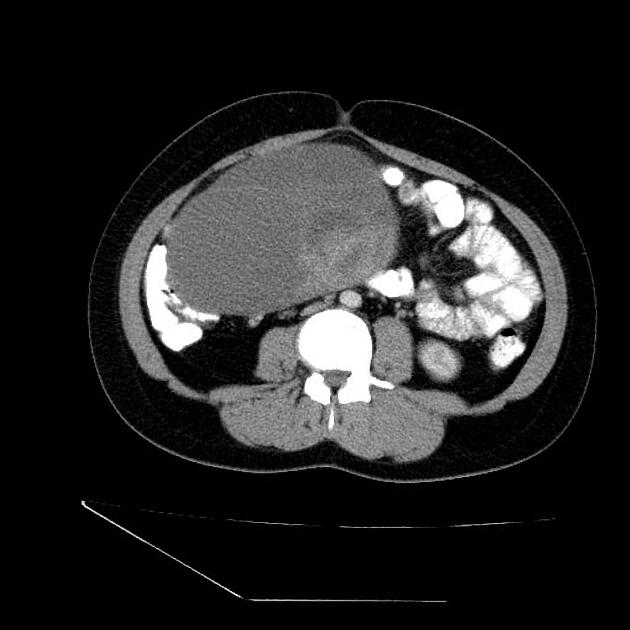
Typical imaging features of ovarian cystadenocarcinoma include:
- cystic adnexal mass with a substantial solid component
- calcification uncommon, but can be seen (~12%) 4
- also seen in serous cystadenoma and other tumors
- frequently bilateral
In the setting of suspected ovarian cystadenocarcinoma, features suggestive of extra-ovarian metastasis include:
- ascites: often of disproportionately large volume 3
- peritoneal nodularity with a high propensity to calcification10
- lymphadenopathy
Ultrasound
- mixed cystic/solid lesion
- more heterogeneous than a serous cystadenoma
- papillary projections, thick septations, and/or solid components
- ascites
- concerning for peritoneal metastatic spread
- discrete peritoneal deposits may be seen
- color Doppler is useful to confirm vascularity of the solid components
- quantitative parameters (resistive index (RI) and pulsatility index (PI)) do not reliably predict malignancy
CT
CT may be used for preoperative evaluation to assess for metastatic disease, e.g. peritoneal nodularity, ascites, or intrathoracic lesions.
MRI
MRI provides the most detailed imaging evaluation for ovarian malignancies and may be used in either preoperative evaluation or post-treatment follow-up.
-
T1
- cystic portions are T1 dark unless there has been intralesional hemorrhage (keep in mind mucinous tumors also have a brighter T1 appearance in the cystic component)
- solid portions are T1 intermediate
-
T2
- cystic portions are T2 bright
- solid portions are T2 intermediate
-
T1 C+ (Gd)
- solid portions enhance
- time-intensity enhancement curves help in risk stratification 11
-
DWI/ADC
- solid components restrict diffusion
- metastases may exhibit restricted diffusion; the cystic components are high T2, low T1 signal unless there has been intralesional hemorrhage (where there is typically slightly increased T1 signal of the cystic component)




















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.