Single photon emission computed tomography (SPECT)
Citation, DOI, disclosures and article data
At the time the article was created Hamish Smith had no recorded disclosures.
View Hamish Smith's current disclosuresAt the time the article was last revised Craig Hacking had the following disclosures:
- Philips Australia, Paid speaker at Philips Spectral CT events (ongoing)
These were assessed during peer review and were determined to not be relevant to the changes that were made.
View Craig Hacking's current disclosures- SPECT
- SPECT/CT
- Single photon emission computed tomography
- SPECTCT
- CT/SPECT
- SPECT-CT
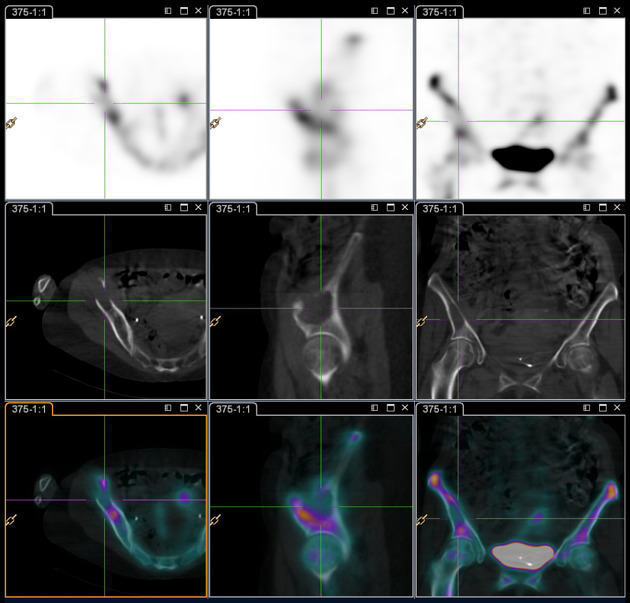
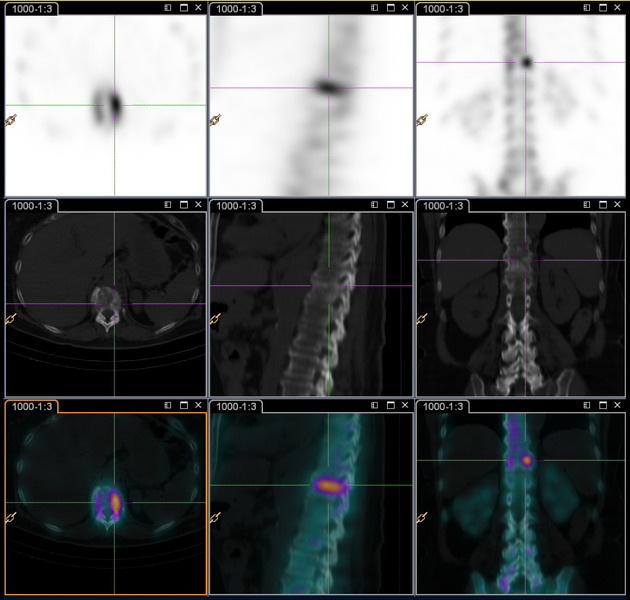
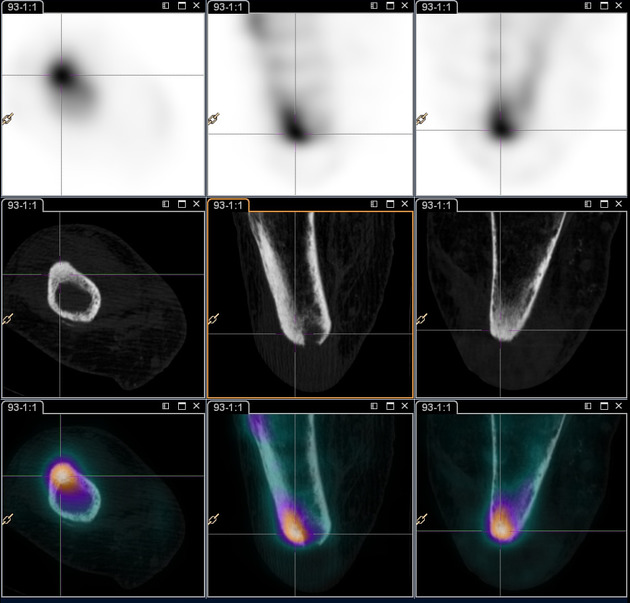
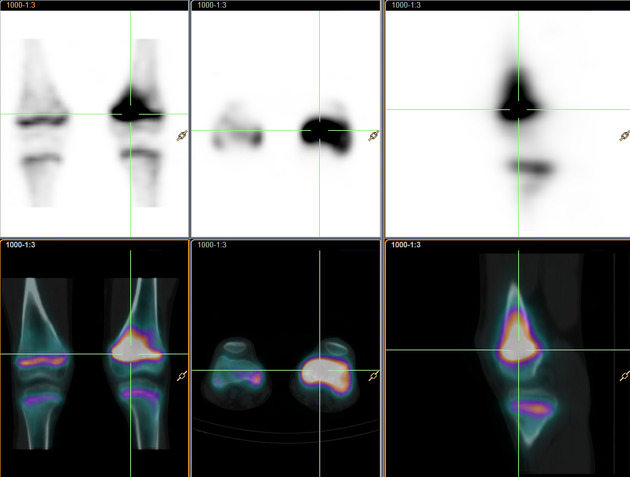
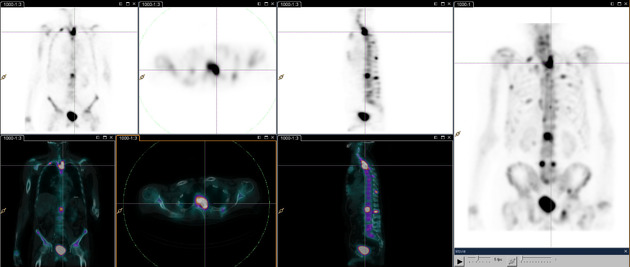
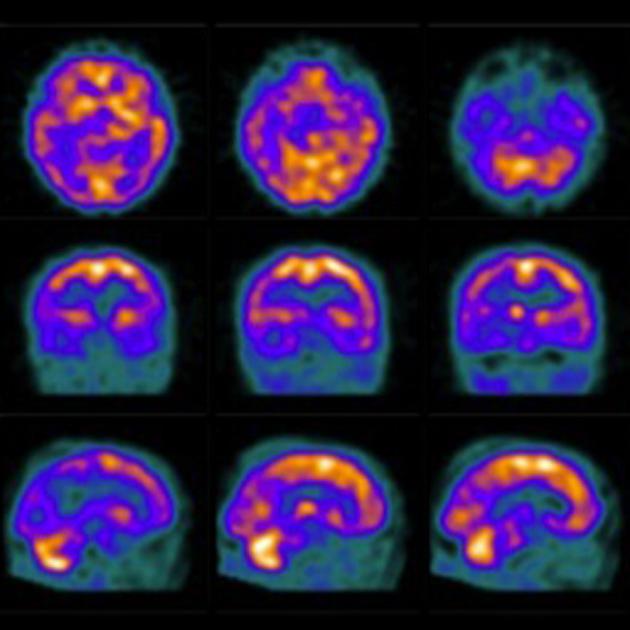
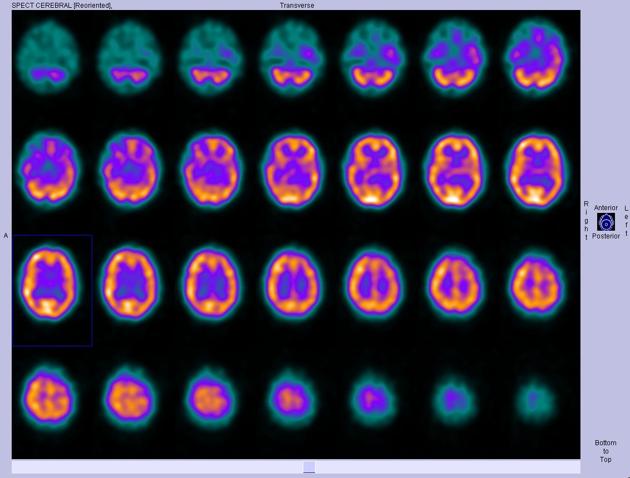
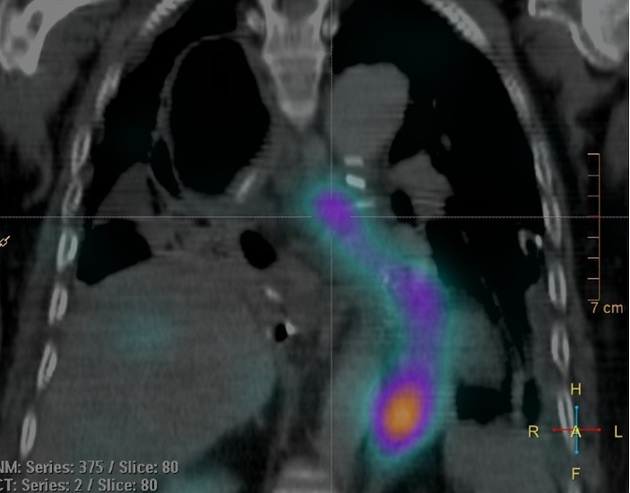
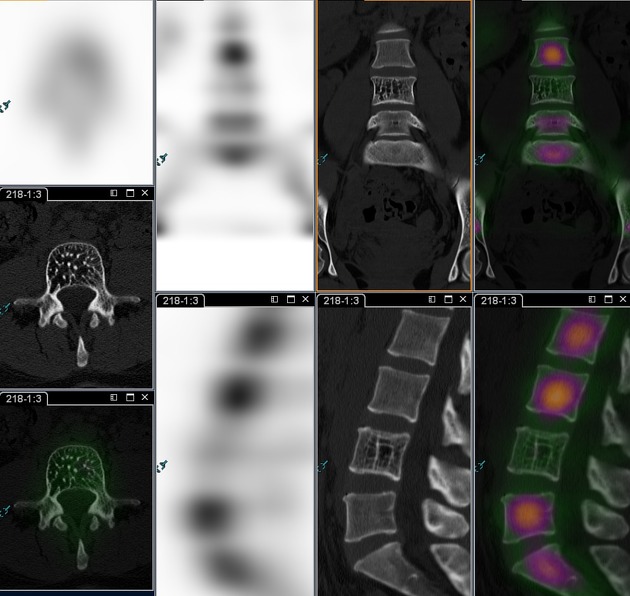
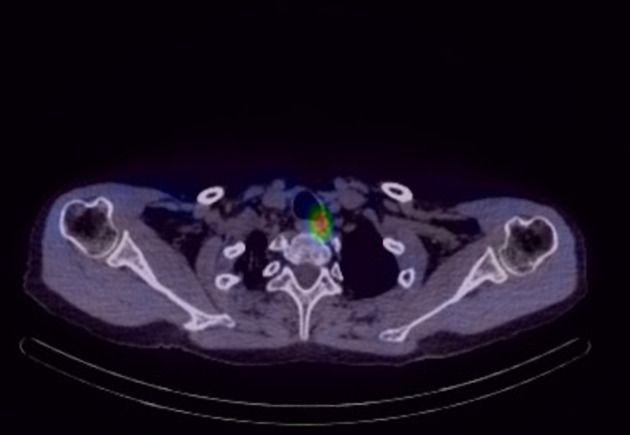
Single photon emission computed tomography (SPECT) is a three-dimensional nuclear medicine imaging technique combining the information gained from scintigraphy with that of computed tomography. This allows the distribution of the radionuclide to be displayed in a three-dimensional manner offering better detail, contrast and spatial information than planar nuclear imaging alone.
SPECT and PET have several similarities but there are major differences which contribute to differing indications, which are discussed here.
On this page:
Design
SPECT machines combine an array of gamma cameras (ranging from one to four cameras) which rotate around the patient on a gantry. SPECT may be also combined with a separate CT machine in a form of hybrid imaging; single photon emission computed tomography-computerized tomography (SPECT-CT) mainly for the purposes of attenuation correction and anatomical localization 1.
ADVERTISEMENT: Supporters see fewer/no ads
Principle
Gamma cameras rotate around the patient providing spatial information on the distribution of the radionuclide within tissues. The use of multiple gamma cameras increases detector efficiency and spatial resolution. The projection data obtained from the cameras are then reconstructed into three-dimensional images usually in axial slices 1-3. When SPECT-CT is used, attenuation correction and higher resolution anatomical localization can be achieved 1.
Uses
brain imaging (perfusion and receptor-binding radiotracers)
Quality control
Upon installation of the SPECT system, tests should be performed to ensure the system functions properly in a proper and stable environment. The sets of tests that should be performed are as below 4:
physical and mechanical inspection of the system
determine the absolute size of a pixel
determine the tomographic uniformity
determine the tomographic resolution in air
determine the tomographic resolution with scatter
determine the offset for center of rotation and alignment of axes
determine slice thickness at the central slice
determine the variations of uniformity and sensitivity with rotation of the system
References
- 1. Roarke MC, Nguyen BD, Pockaj BA. Applications of SPECT/CT in nuclear radiology. (2008) AJR. American journal of roentgenology. 191 (3): W135-50. doi:10.2214/AJR.07.3564 - Pubmed
- 2. Hutton BF. The origins of SPECT and SPECT/CT. (2014) European journal of nuclear medicine and molecular imaging. 41 Suppl 1: S3-16. doi:10.1007/s00259-013-2606-5 - Pubmed
- 3. Tsui BM. The AAPM/RSNA physics tutorial for residents. Physics of SPECT. (1996) Radiographics : a review publication of the Radiological Society of North America, Inc. 16 (1): 173-83. doi:10.1148/radiographics.16.1.173 - Pubmed
- 4. INTERNATIONAL ATOMIC ENERGY AGENCY, Quality Assurance for SPECT Systems, IAEA Human Health Series No. 6, IAEA, Vienna (2009). International Atomic Energy Agency
Incoming Links
- Posterior cortical atrophy
- Lymphoscintigraphy
- Hybrid imaging
- Metastable state
- Tc-99m DMSA
- Radiopharmaceuticals
- Hibernating myocardium
- Gallium-67 scintigraphy
- Cingulate island sign
- Medical abbreviations and acronyms (S)
- SPECT vs PET
- Cerebellar ataxia with neuropathy and vestibular areflexia syndrome (CANVAS)
- Ioflupane (I-123)
- Renal imaging in nuclear medicine
- Cardiac imaging planes
- Anorexia nervosa (CNS manifestations)
- Cyclotron
- Gamma camera
- Bronchopleural fistula
- Gallium-68 DOTATATE
Related articles: Imaging technology
- imaging technology
- imaging physics
- imaging in practice
-
x-rays
- x-ray physics
- x-ray in practice
- x-ray production
- x-ray tube
- filters
- automatic exposure control (AEC)
- beam collimators
- grids
- air gap technique
- cassette
- intensifying screen
- x-ray film
- image intensifier
- digital radiography
- digital image
- mammography
- x-ray artifacts
- radiation units
- radiation safety
- radiation detectors
- fluoroscopy
-
computed tomography (CT)
- CT physics
- CT in practice
- CT technology
- CT image reconstruction
- CT image quality
- CT dose
-
CT contrast media
-
iodinated contrast media
- agents
- water soluble
- water insoluble
- vicarious contrast material excretion
- iodinated contrast media adverse reactions
- agents
- non-iodinated contrast media
-
iodinated contrast media
-
CT artifacts
- patient-based artifacts
- physics-based artifacts
- hardware-based artifacts
- ring artifact
- tube arcing
- out of field artifact
- air bubble artifact
- helical and multichannel artifacts
- CT safety
- history of CT
-
MRI
- MRI physics
- MRI in practice
- MRI hardware
- signal processing
-
MRI pulse sequences (basics | abbreviations | parameters)
- T1 weighted image
- T2 weighted image
- proton density weighted image
- chemical exchange saturation transfer
- CSF flow studies
- diffusion weighted imaging (DWI)
- echo-planar pulse sequences
- fat-suppressed imaging sequences
- gradient echo sequences
- inversion recovery sequences
- metal artifact reduction sequence (MARS)
-
perfusion-weighted imaging
- techniques
- derived values
- saturation recovery sequences
- spin echo sequences
- spiral pulse sequences
- susceptibility-weighted imaging (SWI)
- T1 rho
- MR angiography (and venography)
-
MR spectroscopy (MRS)
- 2-hydroxyglutarate peak: resonates at 2.25 ppm
- alanine peak: resonates at 1.48 ppm
- choline peak: resonates at 3.2 ppm
- citrate peak: resonates at 2.6 ppm
- creatine peak: resonates at 3.0 ppm
- functional MRI (fMRI)
- gamma-aminobutyric acid (GABA) peak: resonates at 2.2-2.4 ppm
- glutamine-glutamate peak: resonates at 2.2-2.4 ppm
- Hunter's angle
- lactate peak: resonates at 1.3 ppm
- lipids peak: resonates at 1.3 ppm
- myoinositol peak: resonates at 3.5 ppm
- MR fingerprinting
- N-acetylaspartate (NAA) peak: resonates at 2.0 ppm
- propylene glycol peak: resonates at 1.13 ppm
-
MRI artifacts
- MRI hardware and room shielding
- MRI software
- patient and physiologic motion
- tissue heterogeneity and foreign bodies
- Fourier transform and Nyquist sampling theorem
- MRI contrast agents
- MRI safety
-
ultrasound
- ultrasound physics
-
transducers
- linear array
- convex array
- phased array
- frame averaging (frame persistence)
- ultrasound image resolution
- imaging modes and display
- pulse-echo imaging
- real-time imaging
-
Doppler imaging
- Doppler effect
- color Doppler
- power Doppler
- B flow
- color box
- Doppler angle
- pulse repetition frequency and scale
- wall filter
- color write priority
- packet size (dwell time)
- peak systolic velocity
- end-diastolic velocity
- resistive index
- pulsatility index
- Reynolds number
- panoramic imaging
- compound imaging
- harmonic imaging
- elastography
- scanning modes
- 2D ultrasound
- 3D ultrasound
- 4D ultrasound
- M-mode
-
ultrasound artifacts
- acoustic shadowing
- acoustic enhancement
- beam width artifact
- reverberation artifact
- ring down artifact
- mirror image artifact
- side lobe artifact
- speckle artifact
- speed displacement artifact
- refraction artifact
- multipath artifact
- anisotropy
- electrical interference artifact
- hardware-related artifacts
- Doppler artifacts
- aliasing
- tissue vibration
- spectral broadening
- blooming
- motion (flash) artifact
- twinkling artifact
- acoustic streaming
- biological effects of ultrasound
- history of ultrasound
-
nuclear medicine
- nuclear medicine physics
- detectors
- tissue to background ratio
-
radiopharmaceuticals
- fundamentals of radiopharmaceuticals
- radiopharmaceutical labeling
- radiopharmaceutical production
- nuclear reactor produced radionuclides
- cyclotron produced radionuclides
- radiation detection
- dosimetry
- specific agents
- carbon-11
- chromium-51
- fluorine agents
- gallium agents
- Ga-67 citrate
- Ga-68
- iodine agents
-
I-123
- I-123 iodide
- I-123 ioflupane (DaTSCAN)
- I-123 ortho-iodohippurate
- I-131
-
MIBG scans
- I-123 MIBG
- I-131 MIBG
-
I-123
- indium agents
- In-111 Octreoscan
- In-111 OncoScint
- In-111 Prostascint
- In-111 oxine labeled WBC
- krypton-81m
- nitrogen-13
- oxygen-15
- phosphorus-32
- selenium-75
-
technetium agents
- Tc-99m DMSA
- Tc-99m DTPA
- Tc-99m DTPA aerosol
- Tc-99m HMPAO
- Tc-99m HMPAO labeled WBC
- Tc-99m MAA
- Tc-99m MAG3
- Tc-99m MDP
- Tc-99m mercaptoacetyltriglycine
- Tc-99m pertechnetate
- Tc-99m labeled RBC
- Tc-99m sestamibi
- Tc-99m sulfur colloid
- Tc-99m sulfur colloid (oral)
- thallium-201 chloride
- xenon agents
- in vivo therapeutic agents
- pharmaceuticals used in nuclear medicine
-
emerging methods in medical imaging
- radiography
- phase-contrast imaging
- CT
- deep-learning reconstruction
- photon counting CT
- virtual non-contrast imaging
- ultrasound
- magnetomotive ultrasound (MMUS)
- superb microvascular imaging
- ultrafast Doppler imaging
- ultrasound localization microscopy
- MRI
- nuclear medicine
- total body PET system
- immuno-PET
- miscellaneous
- radiography






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.