Acute hypersensitivity pneumonitis, also known as acute extrinsic allergic alveolitis, is a legacy term not recommended in the guidelines (c. 2020) 9. It refers to the episodic form of this condition usually happening in just a few hours after the antigen exposure and often recurring with the re-exposure. It represents the most inflammatory side of the spectrum of hypersensitivity pneumonitis and has the potential to resolve with treatment.
On this page:
Terminology
Although the symptomatic disease has been classically divided into acute, subacute, and chronic types, given contradictory definitions on what exactly constitutes each phase, the condition is subtyped into non-fibrotic hypersensitivity pneumonitis and fibrotic hypersensitivity pneumonitis 9.
Clinical presentation
Fever, chills, myalgia, headaches, coughing, chest tightness, dyspnea, and leukocytosis can occur in various combinations and typically occurs 4-12 hours after exposure 1-3.
The symptoms may begin after patients return to an environment from which they have been absent for a while (e.g. resuming work following weekends or holidays) but in at times do not develop with uninterrupted, routine contact with the same antigen.
Pathology
Microscopic appearance
Acute hypersensitivity pneumonitis is histologically characterized by the presence of neutrophilic infiltration of the respiratory bronchioles and alveoli. A pattern of diffuse alveolar damage and temporally uniform, non-specific, chronic interstitial pneumonitis may also be seen.
Radiographic features
Plain radiograph
Chest radiographs are often normal in patients with mild symptoms and can remain normal despite severe symptoms 3.
When abnormal, it may present with:
bilateral areas of increased opacities that may be either heterogeneous or homogeneous and can simulate pulmonary edema 2,3
numerous poorly defined small (<5 mm) opacities throughout both lungs, sometimes with sparing of the apices and bases
a pattern of fine reticulation may also occur
zonal distribution is variable from patient to patient and may even show temporal variation within the same patient
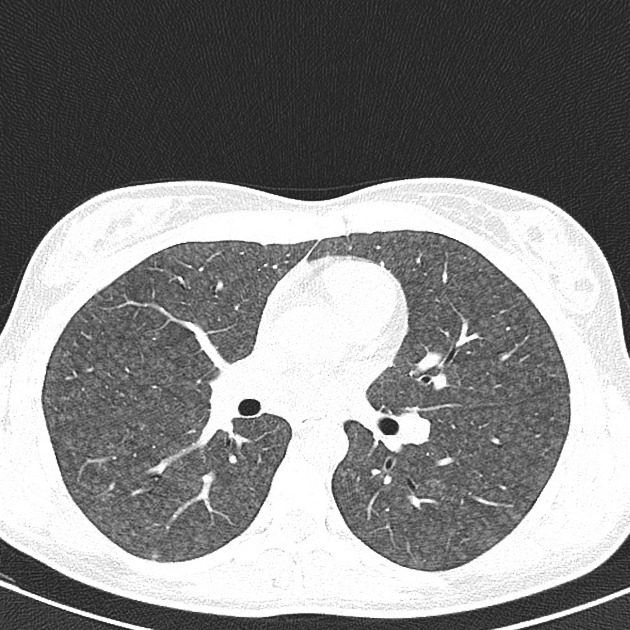
CT
The acute phase is dominated by air space abnormality (alveolitis) with no features of fibrosis. Findings include:
homogeneous groundglass opacities that are usually bilateral and symmetric, but sometimes patchy and concentrated in the middle part and base of the lungs or in a bronchovascular distribution
numerous "soft" centrilobular opacities: usually <5 mm in diameter (occasionally these opacities have well-defined borders and soft-tissue attenuation)
hypoattenuation and hypovascularity of scattered secondary lobules: hypoattenuating regions that persist on expiratory CT scans are indicative of air trapping, which is caused by bronchiolar inflammation and obstruction: this may give a mosaic attenuation pattern
there may be a lower zonal predilection in the acute form







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.