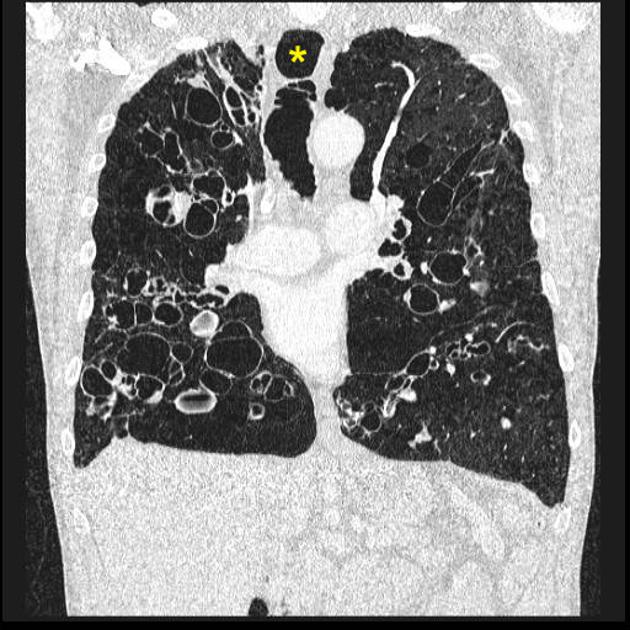
Tracheobronchomegaly, also known as Mounier-Kuhn syndrome, is a rare condition characterized by markedly dilated trachea and central airways, with recurrent infection.
On this page:
Epidemiology
Mounier-Kuhn syndrome is most frequently seen in middle-aged men before the age of 50 years 1,6.
Clinical presentation
The anatomical and physiological changes in the airways predispose to stagnation within enlarged portions of the bronchial tree. Chronic productive cough and recurrent pulmonary infections are common 1,2. Clinical features may mimic and co-exist with COPD 4.
It is unclear whether Mounier-Kuhn syndrome is a distinct entity or simply tracheobronchomegaly in the setting of underlying primary abnormalities. If the latter definition is used, associations include connective tissue disorders such as 2,6:
Pathology
The underlying abnormality is an absence or marked atrophy of the elastic fibers and smooth muscle within the wall of the trachea and main bronchi. While likely congenital, this has not been established.
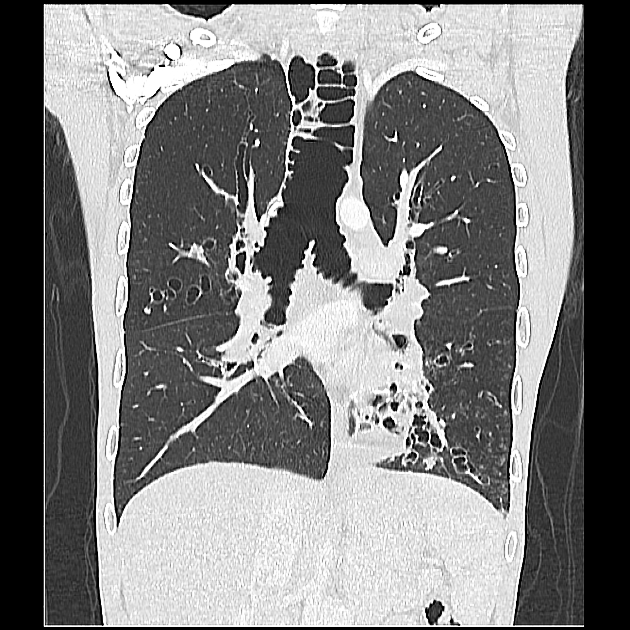
The airway walls are thin and flaccid, resulting in significant change in airway caliber during respiration. In inspiration, negative intra-thoracic pressure markedly enlarges the trachea. In expiration, the reversed intra-thoracic pressure causes collapse. Bronchial and tracheal diverticulosis between the cartilaginous rings, and bronchiectasis, are common 2.
The bronchial myenteric plexus is absent 2.
Radiographic features
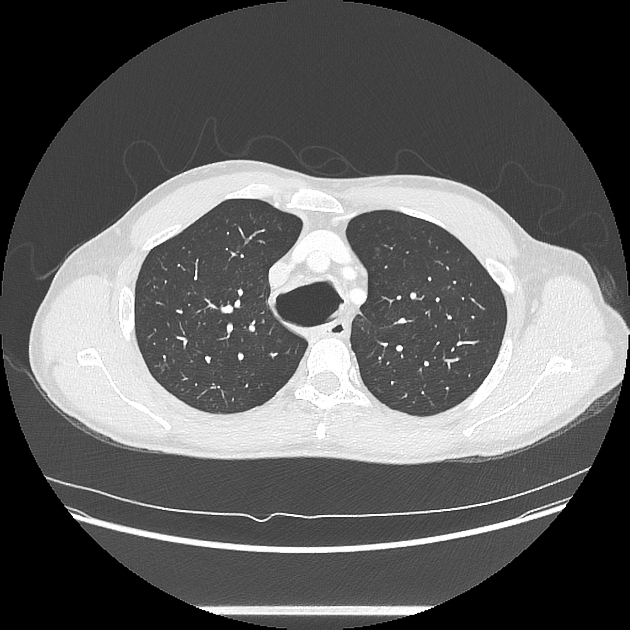
The most sensitive imaging test is a biphasic CT with images of the trachea obtained during inspiration and expiration. Two-phase chest radiographs will also demonstrate the enlargement of the trachea on inspiration and collapse during expiration, but they are clearly less sensitive.
To consider the diagnosis, the diameter of the trachea should be greater than 3 cm: this is usually measured 2 cm above the aortic arch 1,2. Other measurements that have been used to make the diagnosis include bronchial diameters of 20 or 24 mm (right), and 15 or 23 mm (left) 2,4.
Posteriorly projecting tracheal diverticula may be seen.
Treatment and prognosis
Treatment is usually conservative with physiotherapy and postural drainage. Acute exacerbations are treated with antibiotics. In rare instances, tracheal stenting has been used 4.
History and etymology
It was initially described by Pierre-Louis Mounier-Kuhn, a French physician, in 1932 3-5.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.