Passive atelectasis
Citation, DOI, disclosures and article data
At the time the article was created Craig Hacking had no recorded disclosures.
View Craig Hacking's current disclosuresAt the time the article was last revised Liz Silverstone had no financial relationships to ineligible companies to disclose.
View Liz Silverstone's current disclosures- Relaxation atelectasis
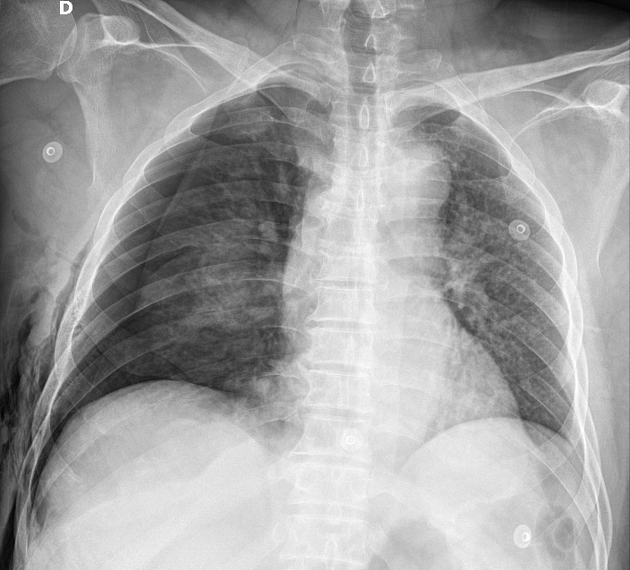
Passive atelectasis, also known as relaxation atelectasis is due to elastic recoil of the lung when normal negative pleural pressure is reduced or lost due to a pleural collection such as a pneumothorax or pleural effusion.
On this page:
Clinical presentation
The clinical presentation would depend on the extent of atelectasis and how quickly it develops. Small and gradually developing areas of atelectasis may be asymptomatic or present as a non-productive cough. Larger areas that develop more quickly can present with hypoxia, respiratory failure, cough, and/or pleuritic chest pain 6.
Physical examination of the lungs may reveal a diminished movement of the affected area, dullness on percussion decreased or absent breath sounds, and ipsilateral tracheal deviation 6.
Pathology
With a loss of the negative intrapleural pressure there is equalization of intrapleural and intra-alveolar pressures and the lung is said to "relax" due to its normal elastic recoil resulting in lung volume loss 5. In the case of diaphragmatic abnormalities, there is a reduction in downward force to fully expand the lungs resulting in passive atelectasis 5.
Etiology
Causes of passive atelectasis may be grouped into three main categories 5:
simple pneumothorax
-
conditions of hypoventilation
chest wall mass
Radiographic features
Plain radiograph
There may not be a significant increase in density from the atelectasis, as perfusion of the affected lung also decreases ref.
CT
atelectatic lung may demonstrate marked enhancement, greater than that of skeletal muscle (see case 2)
the presence of air bronchograms helps to exclude airway obstruction as a cause
as gases are the main constituent of normal lung, loss of aeration can cause profound collapse
Quiz questions
References
- 1. W. Richard Webb, Charles B. Higgins. Thoracic Imaging. (2011) ISBN: 9781605479767 - Google Books
- 2. Vinay Kumar, Abul K. Abbas, Jon C. Aster. Robbins & Cotran Pathologic Basis of Disease. (2020) ISBN: 9780323531139 - Google Books
- 3. Richard B. Gunderman. Essential Radiology. (2006) ISBN: 9781588900821 - Google Books
- 4. Ray K, Bodenham A, Paramasivam E. Pulmonary Atelectasis in Anaesthesia and Critical Care. Continuing Education in Anaesthesia Critical Care & Pain. 2014;14(5):236-45. doi:10.1093/bjaceaccp/mkt064
- 5. Woodring J & Reed J. Types and Mechanisms of Pulmonary Atelectasis. J Thorac Imaging. 1996;11(2):92-108. doi:10.1097/00005382-199621000-00002 - Pubmed
- 6. Al-Tubaikh J. Atelectasis (Lung Collapse). Intern Med. 2010;:119-22. doi:10.1007/978-3-642-03709-2_20
Incoming Links
- Pneumothorax
- Hepatic abscesses and large splenic abscess
- Catamenial pneumothorax
- Kidney injury due to fall
- Small bowel obstruction due to wandering gastrostomy tube
- Clostridioides difficile colitis
- Ivor Lewis esophagectomy complication
- Pleural sarcomatoid mesothelioma
- Delayed traumatic splenic rupture
- Massive aortic aneurysm, dissection and pericardial effusion
Related articles: Airspace opacification
- airspace opacification
- differential diagnoses of airspace opacification[+][+]
- lobar consolidation[+][+]
-
atelectasis
-
mechanism-based
- resorptive (obstructive) atelectasis
- passive (relaxation) atelectasis
- compressive atelectasis
- cicatrisation atelectasis
- adhesive atelectasis
- gravity dependant atelectasis
- morphology-based[+][+]
-
mechanism-based
- lobar lung collapse[+][+]
Related articles: Chest
- imaging techniques
-
chest radiograph
- radiography[+][+]
-
approach
- ABCDE
- ABCDEFGHI
- congenital heart disease
- medical devices in the thorax
- common lines and tubes[+][+]
- nasogastric tubes
- endotracheal tubes
- central venous catheters
- esophageal temperature probe
- tracheostomy tube
- pleural catheters
- cardiac conduction devices
- prosthetic heart valve
- review areas
-
airspace opacification
- differential diagnoses of airspace opacification[+][+]
- lobar consolidation[+][+]
-
atelectasis
-
mechanism-based
- resorptive (obstructive) atelectasis
- passive (relaxation) atelectasis
- compressive atelectasis
- cicatrisation atelectasis
- adhesive atelectasis
- gravity dependant atelectasis
- morphology-based[+][+]
-
mechanism-based
- lobar lung collapse[+][+]
- chest x-ray in the exam setting[+][+]
- cardiomediastinal contour[+][+]
- chest radiograph zones[+][+]
- tracheal air column[+][+]
- fissures[+][+]
- normal chest x-ray appearance of the diaphragm[+][+]
- nipple shadow[+][+]
-
lines and stripes[+][+]
- anterior junction line
- posterior junction line
- right paratracheal stripe
- left paratracheal stripe
- posterior tracheal stripe/tracheo-esophageal stripe
- posterior wall of bronchus intermedius
- right paraspinal line
- left paraspinal line
- aortic-pulmonary stripe
- aortopulmonary window
- azygo-esophageal recess
- spaces[+][+]
- signs[+][+]
- air bronchogram
- big rib sign
- Chang sign
- Chen sign
- coin lesion
- continuous diaphragm sign
- dense hilum sign
- double contour sign
- egg-on-a-string sign
- extrapleural sign
- finger in glove sign
- flat waist sign
- Fleischner sign
- ginkgo leaf sign
- Golden S sign
- Hampton hump
- haystack sign
- hilum convergence sign
- hilum overlay sign
- Hoffman-Rigler sign
- holly leaf sign
- incomplete border sign
- juxtaphrenic peak sign
- Kirklin sign
- medial stripe sign
- melting ice cube sign
- more black sign
- Naclerio V sign
- Palla sign
- pericardial fat tag sign
- Shmoo sign
- silhouette sign
- snowman sign
- spinnaker sign
- steeple sign
- straight left heart border sign
- third mogul sign
- tram-track sign
- walking man sign
- water bottle sign
- wave sign
- Westermark sign
- HRCT[+][+]
-
chest radiograph
- airways[+][+]
- bronchitis
- small airways disease
-
bronchiectasis
- broncho-arterial ratio
- related conditions
- differentials by distribution
- narrowing
-
tracheal stenosis
- diffuse tracheal narrowing (differential)
-
bronchial stenosis
- diffuse airway narrowing (differential)
-
tracheal stenosis
- diverticula
- pulmonary edema[+][+]
-
interstitial lung disease (ILD)[+][+]
- Anti-Jo-1 antibody-positive interstitial lung disease
- drug-induced interstitial lung disease
-
hypersensitivity pneumonitis
- acute hypersensitivity pneumonitis
- subacute hypersensitivity pneumonitis
- chronic hypersensitivity pneumonitis
- etiology
- bird fancier's lung: pigeon fancier's lung
- farmer's lung
- cheese workers' lung
- bagassosis
- mushroom worker’s lung
- malt worker’s lung
- maple bark disease
- hot tub lung
- wine maker’s lung
- woodsman’s disease
- thatched roof lung
- tobacco grower’s lung
- potato riddler’s lung
- summer-type pneumonitis
- dry rot lung
- machine operator’s lung
- humidifier lung
- shower curtain disease
- furrier’s lung
- miller’s lung
- lycoperdonosis
- saxophone lung
-
idiopathic interstitial pneumonia (mnemonic)
- acute interstitial pneumonia (AIP)
- cryptogenic organizing pneumonia (COP)
- desquamative interstitial pneumonia (DIP)
- non-specific interstitial pneumonia (NSIP)
- idiopathic pleuroparenchymal fibroelastosis
- lymphoid interstitial pneumonia (LIP)
- respiratory bronchiolitis–associated interstitial lung disease (RB-ILD)
- usual interstitial pneumonia / idiopathic pulmonary fibrosis (UIP/IPF)
-
pneumoconioses
- fibrotic
- non-fibrotic
-
lung cancer[+][+]
-
non-small-cell lung cancer
-
adenocarcinoma
- pre-invasive tumors
- minimally invasive tumors
- invasive tumors
- variants of invasive carcinoma
- described imaging features
- adenosquamous carcinoma
- large cell carcinoma
- primary sarcomatoid carcinoma of the lung
- squamous cell carcinoma
- salivary gland-type tumors
-
adenocarcinoma
- pulmonary neuroendocrine tumors
- preinvasive lesions
-
lung cancer invasion patterns
- tumor spread through air spaces (STAS)
- presence of non-lepidic patterns such as acinar, papillary, solid, or micropapillary
- myofibroblastic stroma associated with invasive tumor cells
- pleural invasion
- vascular invasion
- tumors by location
- benign neoplasms
- pulmonary metastases
- lung cancer screening
- lung cancer staging
-
non-small-cell lung cancer






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.