Left atrial enlargement (LAE) may result from many conditions, either congenital or acquired. It has some characteristic findings on a frontal chest radiograph. CT or MRI may also be used for diagnosis.
On this page:
Clinical presentation
An enlarged left atrium can have many clinical implications, such as:
Ortner syndrome: left recurrent laryngeal nerve palsy secondary to compression from enlarged left atrium
dysphagia megalatriensis: compression of esophagus between the enlarged left atrium and vertebral bodies
atrial fibrillation: via a multiple wavelet mechanism
thromboembolic events (e.g. ischemic stroke): due to stasis of blood in the enlarged left atrium (especially the left atrial appendage) and/or atrial fibrillation
Pathology
Broadly speaking, the causes of left atrial enlargement can be divided into congenital and acquired causes:
-
acquired
-
it is uncertain if this is a cause or only a consequence 10
-
congenital
The common mechanism is increased atrial wall tension due to increased filling pressures, which eventually leads to atrial enlargement.
There are associations between left atrial enlargement and atrial fibrillation, stroke, and mortality after myocardial infarction. With a reduced incidence of mitral valve disease from rheumatic fever, the incidence of left atrial enlargement has also decreased.
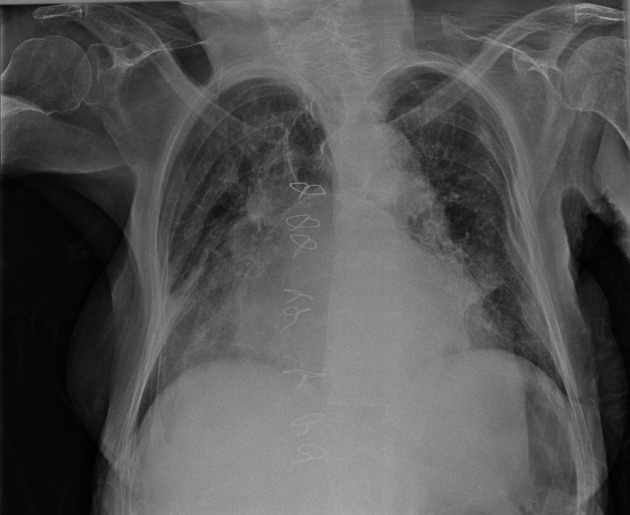
Radiographic features
Cardiac chamber enlargement is typically assessed volumetrically with echocardiography, but can also be assessed (although less widespread) with CT and MRI. Chest x-rays, however, are so frequently obtained, and formed the mainstay of chest imaging for decades, that a great deal has been written about the various appearances of chamber enlargement. It is, therefore, essential to be familiar with normal cardiomediastinal outlines.
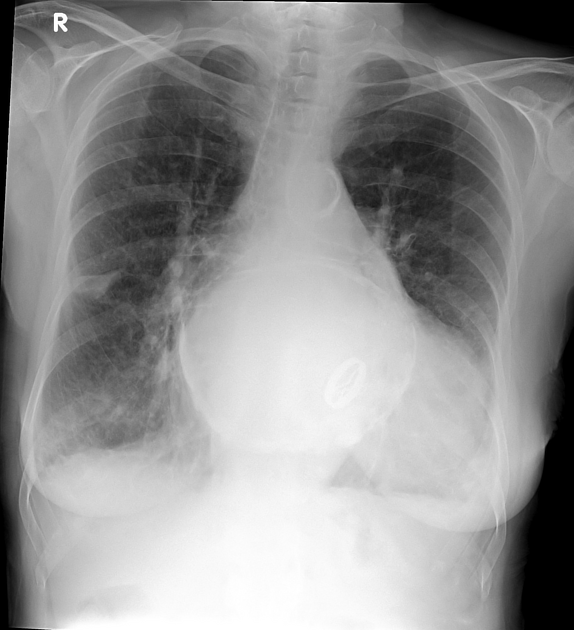
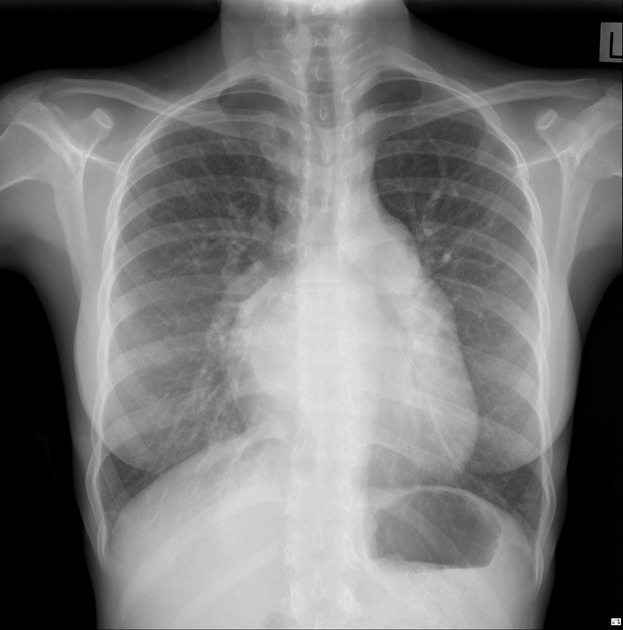
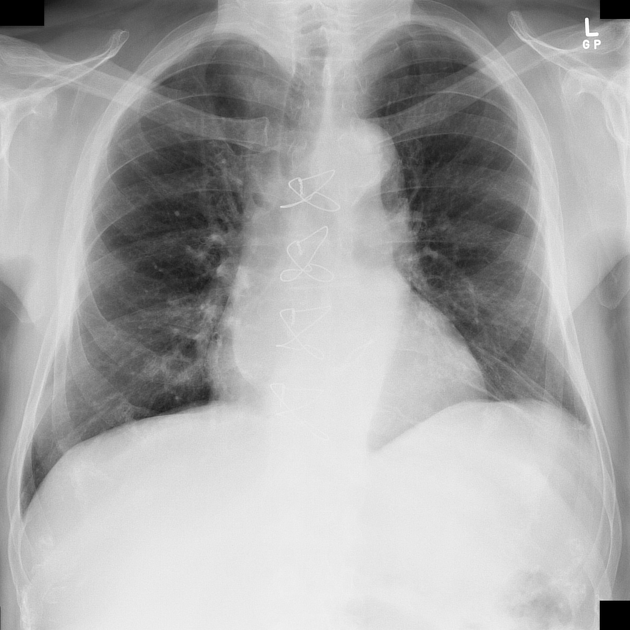
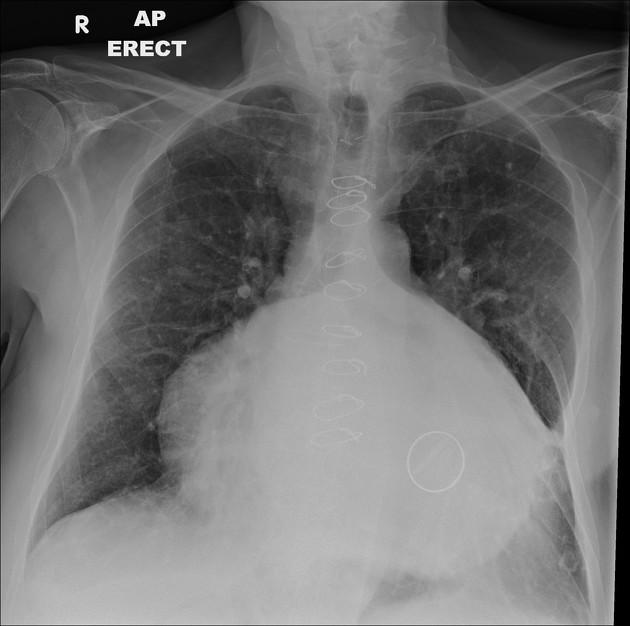
Plain radiograph
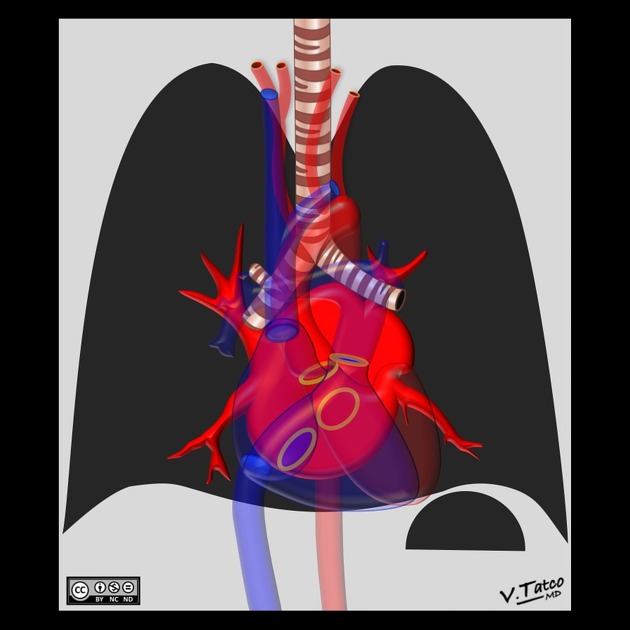
As the left atrium enlarges, it may become directly visible, or displace adjacent structures.
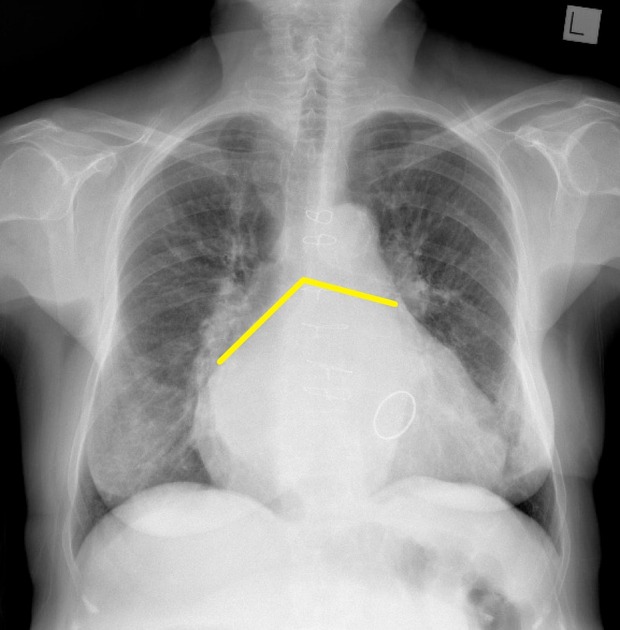
Direct visualization of the enlarged atrium includes:
-
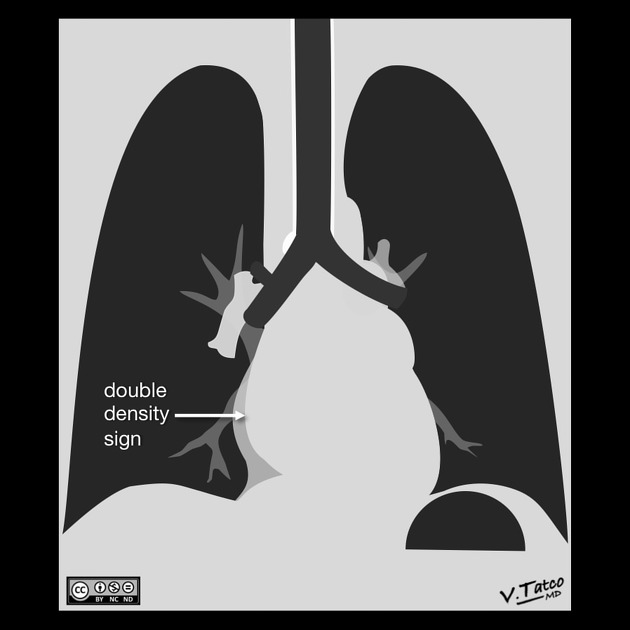
when the right side of the left atrium pushes into the adjacent lung, and becomes visible superimposed or even beyond the normal right heart border (known as atrial escape)
a similar appearance can be caused by the right superior pulmonary vein in patients without atrial enlargement 4
-
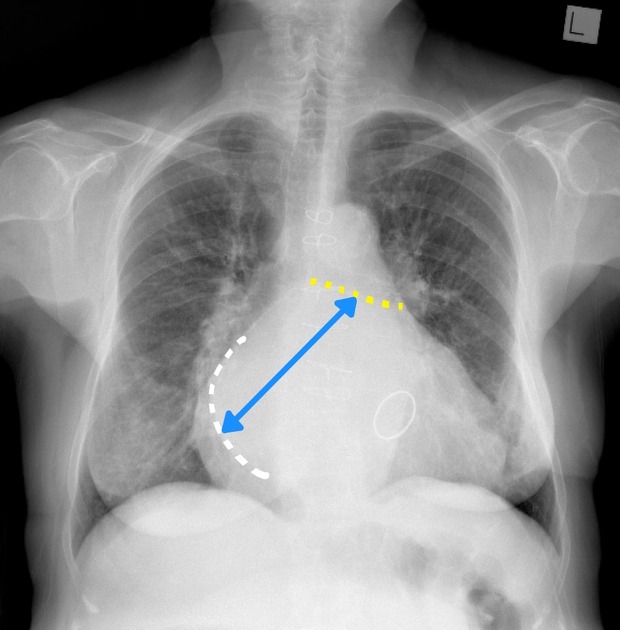
oblique measurement of greater than 7 cm 5,6
measured from midpoint of left main bronchus to the right border of the left atrium (this requires a double density sign of course)
thought to be the most reliable sign on chest radiography
convex left atrial appendage (third mogul sign): normally the left heart border just below the pulmonary outflow track should be flat or slightly concave
Indirect signs include:
-
splaying of the carina, with the increase of the tracheal bifurcation angle to over 90 degrees
this refers to both the interbronchial angle (i.e. angle formed by the central axis of the left and right main bronchi) and the subcarinal angle 1-3
both are inaccurate and dependent on radiographer technique, inspiration and body habitus 2
-
the mean and range of both measurements vary widely in normal individuals 2,3
interbronchial angle: normal mean 67-77° (range 34-109°)
subcarinal angle: normal mean 62-73° (range 34-90°)
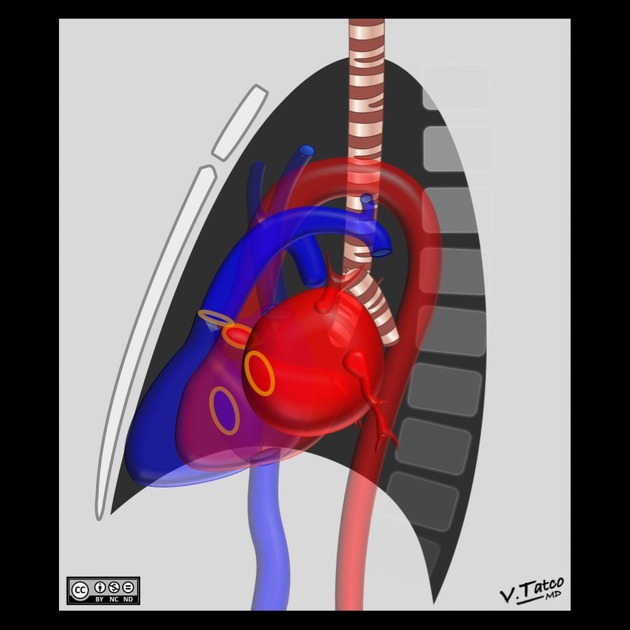
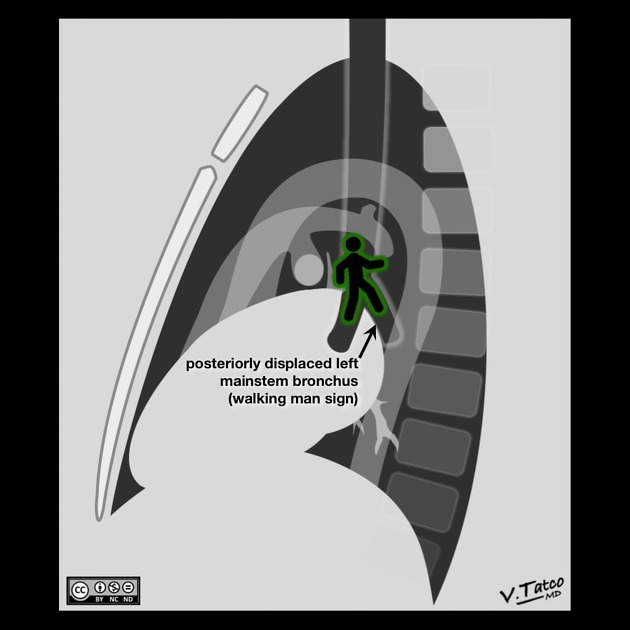
-
posterior displacement of the left mainstem bronchus on the lateral radiograph
right and left bronchi, therefore, do not overlap, but rather form an upside down 'V', sometimes referred to as the walking man sign 5
superior displacement of the left mainstem bronchus on frontal view
posterior displacement of a barium-filled esophagus or nasogastric tube
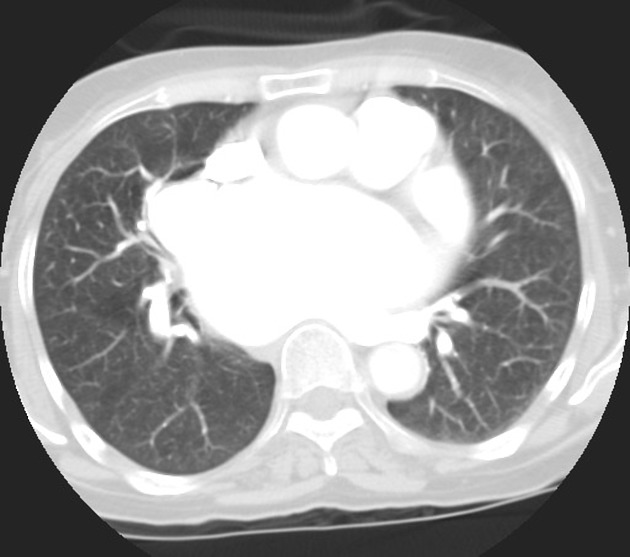
CT and MRI
CT and MRI measurements of the left atrium rely on echocardiography data 7. Measurement is made at end ventricular systole when the left atrium is the maximum size.
-
normal left atrial AP diameter
women: <4.0 cm
men: <4.1 cm
An accurate AP measurement is made on the three-chamber view on a gated cardiac CT. The AP left atrial diameter on a non-gated contrast-enhanced CT can only be an estimate since foreshortening of the chamber and the cardiac cycle cannot be accounted for.
Atrial volume measurements are considered more accurate than either AP or area measurements. The atrial volume can be calculated with: 8/3π[(area of the four chamber view)*(area of the two chamber view)/(shortest inferior-superior length from the annular plane to the back wall of the atrium)]
-
normal atrial volume
women: <53 mL
men: <59 mL
One thing to remember is that echocardiography data for left atrial enlargement slightly underestimates the volume of the left atrium made by CT, so one must be careful not to overcall mild left atrial enlargement on CT 8.
ECG
ECG Criteria for left atrial enlargement include:
total P wave duration >110 ms in lead II11
P mitrale (broad, bifid P wave with inter-peak duration >40 ms) in lead II11
biphasic P wave with terminal negative portion > 40 ms duration in lead V111
biphasic P wave with terminal negative portion > 1mm deep in lead V111
Echocardiography
Transthoracic measurements of left atrial volume represent one of the most robust indices of cardiovascular disease; left atrial remodeling and enlargement occurs as a function of the chronicity and degree of elevated filling pressures, and are a strong predictor of cardiovascular mortality.
Previously accepted linear measurements from the parasternal long and apical 4 chamber views used to derive area using the ellipsoid model are now discouraged. The disk summation model is now the standard for measurement, akin to Simpson's method of disks to derive left ventricular volumes. Left atrial volume can be calculated at end-systole in the apical 4 and 2 chamber views, racing the endocardial border of the left atrium, excluding the pulmonary vein inlet and the area enclosed within the mitral valve annulus. Using body surface area, an index LA volume is resulted, with a recommended upper limit of normal being an indexed left atrial volume of 34 mL/m2 7.
Practical points
left atrial enlargement is associated with thrombus formation (check the left atrial appendage)













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.