Bronchiectasis is irreversible dilatation of the bronchial tree, and is commonly accompanied by bronchial wall thickening and mucoid impaction 25.
On this page:
Terminology
If reversibility is uncertain use the term “bronchial dilatation” 25.
The term bronchiolectasis refers to irreversible dilatation of distal non-cartilaginous airways.
Traction bronchiectasis refers to bronchial dilatation caused by fibrosis and is associated with irregular wall thickening 25.
Traction bronchiolectasis refers to dilatation of the non-cartilaginous airways in the central secondary pulmonary lobule which normally measure <2 mm and is typically associated with honeycombing and caused by fibrosis 25.
The plural of bronchiectasis is “bronchiectases” however this term is rarely used.
Epidemiology
The incidence of bronchiectasis is difficult to gauge; infection is the most common cause and the disease is more common in low socioeconomic groups. Globally, infectious diseases account for about 30% of cases and in a similar proportion the cause is unknown. Tuberculosis accounts for about 14% and cystic fibrosis, chronic obstructive pulmonary disease (COPD) and asthma make a minor contribution 26.
Diagnosis
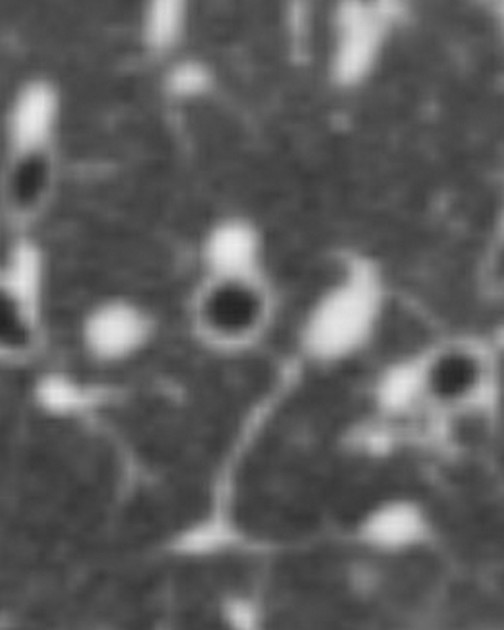
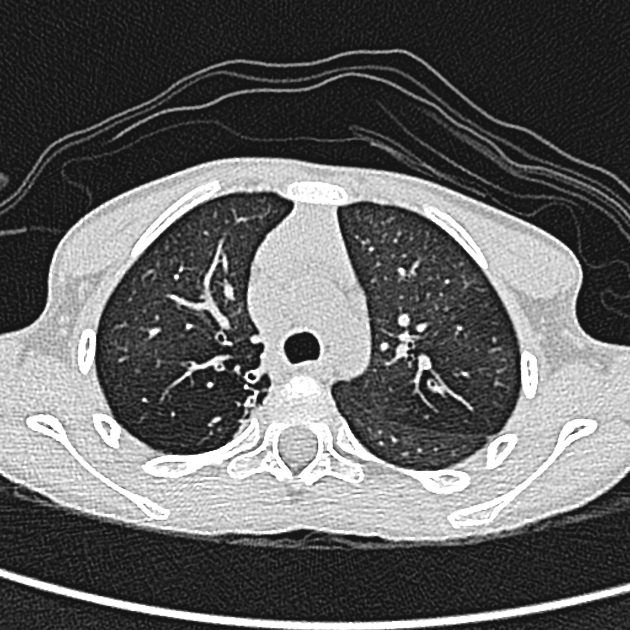
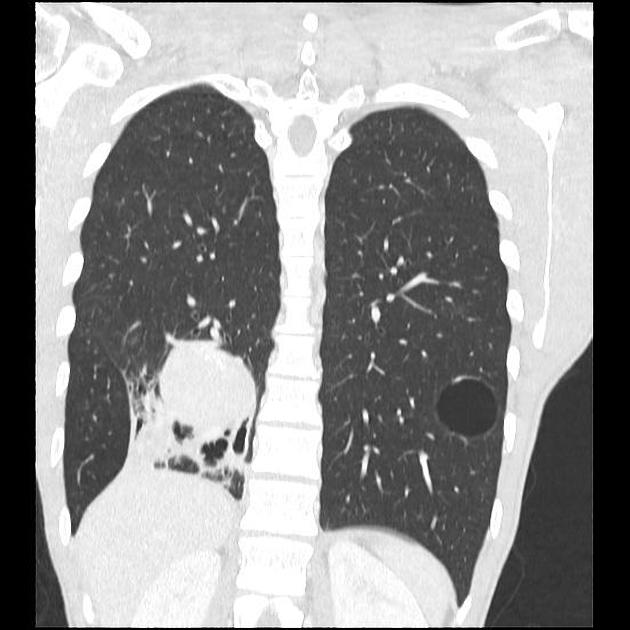
Bronchial dilatation is present if the bronchial diameter exceeds the diameter of the accompanying pulmonary artery on CT (signet ring sign). Absence of normal tapering and abnormal visualization of peripheral airways within 1 cm of the pleural surface are common signs of bronchiectasis 25. Thickened bronchial walls and adjacent scarring are common. Irreversibility must be established to distinguish bronchiectasis from bronchial dilatation.
Clinical presentation
Bronchiectasis can present with recurrent chest infections, chronic or recurrent productive cough, hemoptysis or cor pulmonale.
Pathology
Dilatation is caused by congenital deficiency or acquired destruction and weakening of the muscular and elastic layers in the bronchial walls. Impaired clearance of secretions predisposes to recurrent infections, obstructions and further damage. Inflammation in surrounding alveoli can lead to peribronchial fibrosis 25,27.
Etiology
Commoner causes include infection, inflammation, congenital and proximal airway obstruction. Causes include 1-7,9,17,21:
idiopathic, i.e. unknown (most common)
-
impaired host defenses
cystic fibrosis (most common cause in children)
primary ciliary dyskinesia, e.g. Kartagener syndrome, Young syndrome
primary immunodeficiency disorder, e.g. common variable immunodeficiency, hypogammaglobulinaemia, chronic granulomatous disease
HIV/AIDS 15,16
-
postinfective (most common known non-cystic fibrosis cause in adults)
bacterial pneumonia and bronchitis, e.g. S. aureus, H. influenzae, B. pertussis
mycobacterial infection, e.g. tuberculosis, Mycobacterium avium-intracellulare complex
-
allergic and autoimmune
connective tissue disease, e.g. rheumatoid arthritis 6, Sjögren syndrome, systemic lupus erythematosus (SLE) 7
-
obstruction
severe obstructive lung disease: asthma or chronic obstructive pulmonary disease (COPD)
neoplasm, e.g. bronchial carcinoid, lung cancer inhaled foreign bodies
-
congenital
bronchial tree malformations, e.g. Mounier-Kuhn syndrome, Williams-Campbell syndrome, pulmonary sequestration, bronchial atresia
-
others
traction bronchiectasis due to diffuse lung disease, e.g. pulmonary fibrosis
post-transplantation
A mnemonic to remember common causes is CAPT Kangaroo has Mounier-Kuhn.
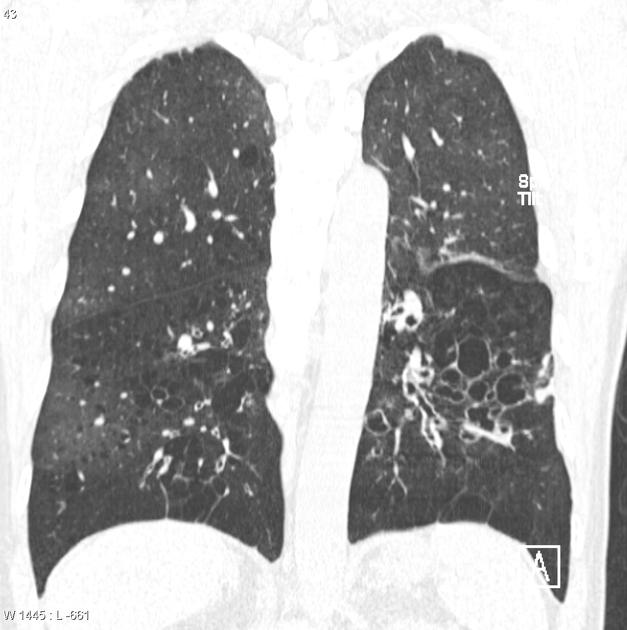
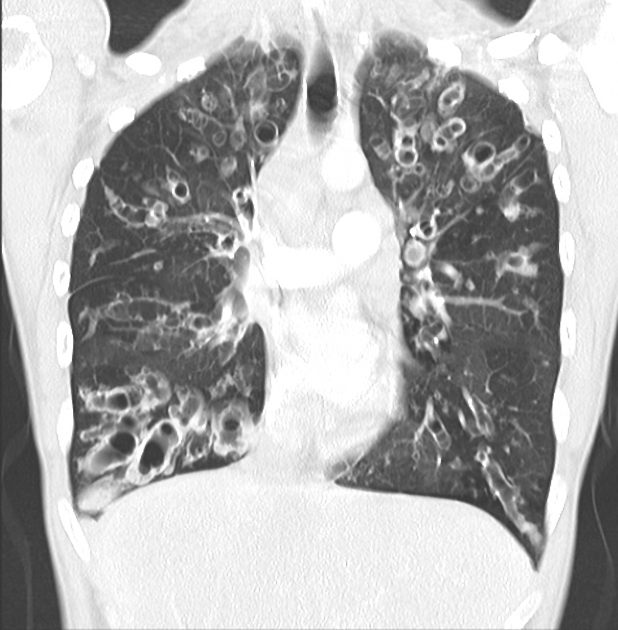
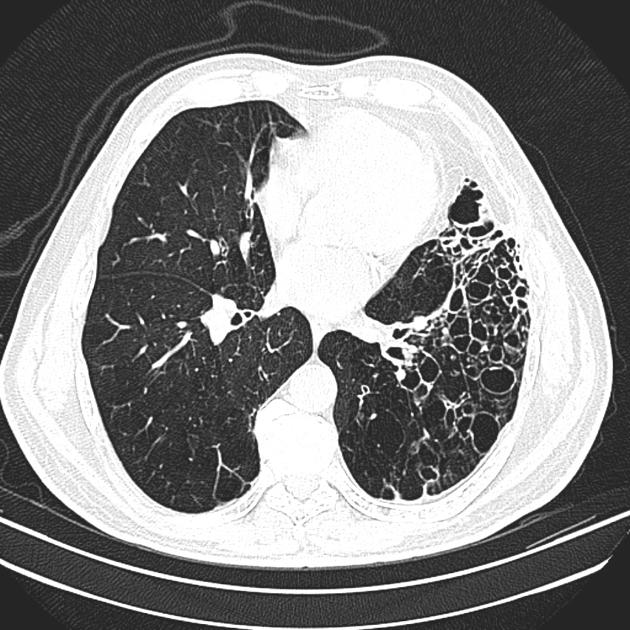
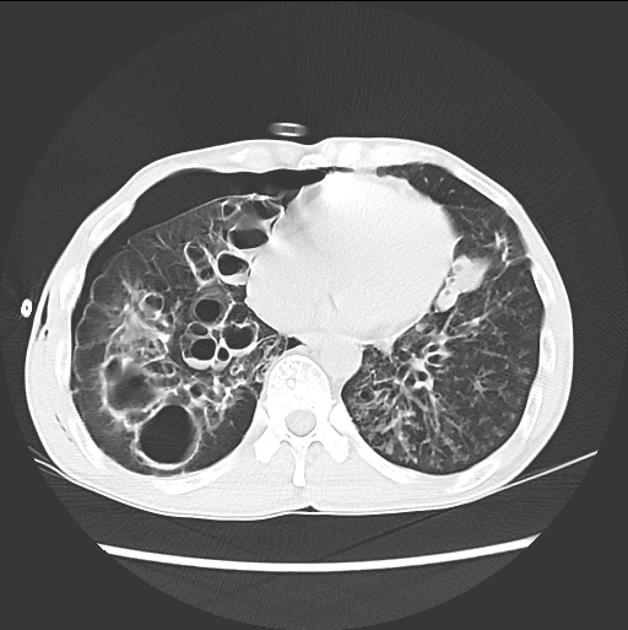
Subtypes
According to macroscopic morphology, three types have been described which reflect chronicity and severity 8:
-
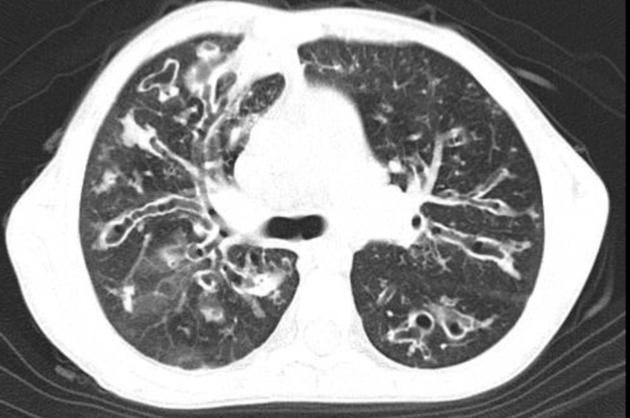
bronchi have a uniform caliber, do not taper and have parallel walls (tram track sign and signet ring sign)
commonest form 14
-
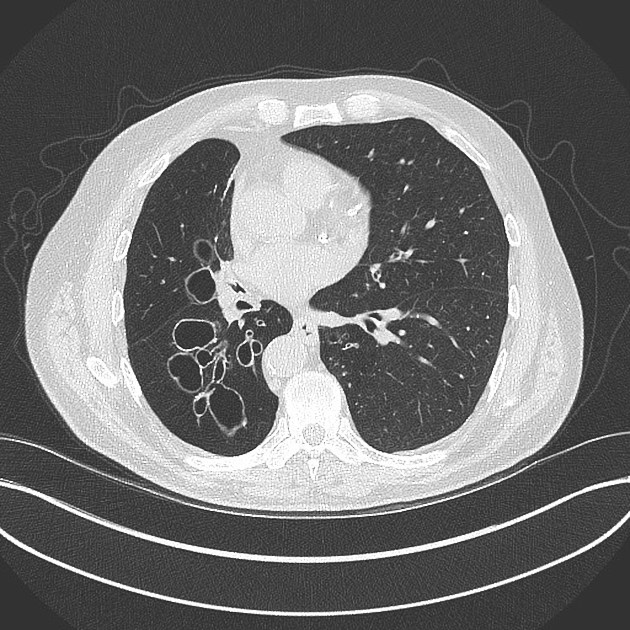
relatively uncommon
beaded appearances where dilated bronchi have interspersed sites of relative narrowing
-
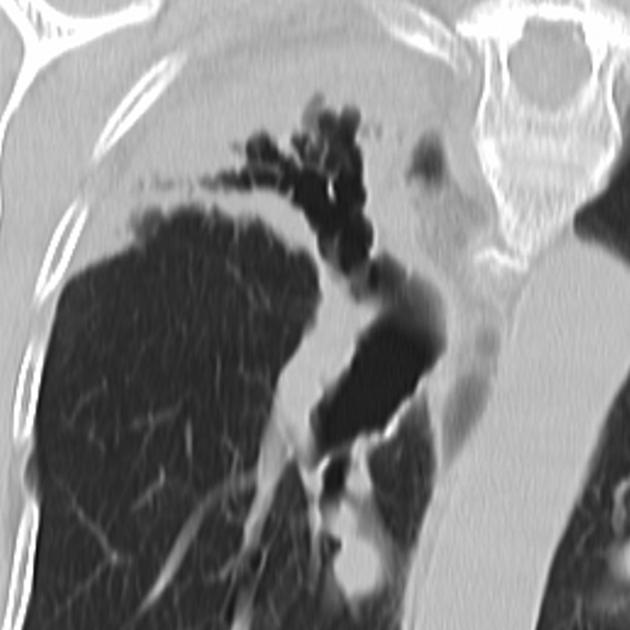
severe form with cyst-like bronchi that extend to the pleural surface
air-fluid levels are commonly present
According to one study, the relative prevalence were 14:
cylindrical: ~45%
varicose: ~10%
cystic: ~ 45%
multiple types: ~25%
Scoring systems
Radiographic features
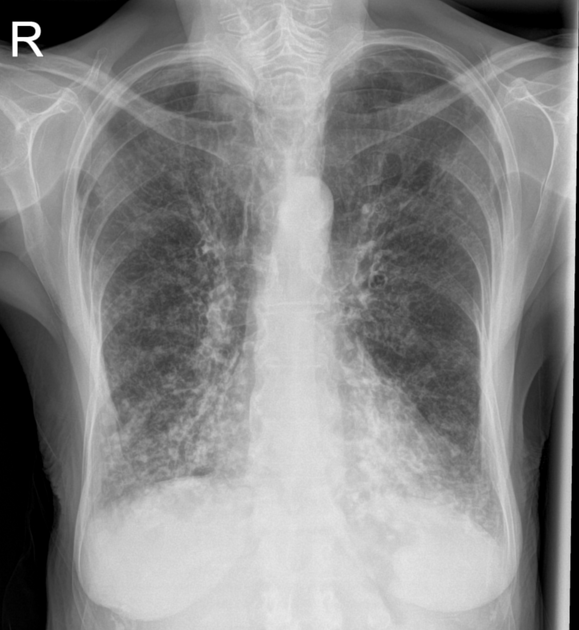
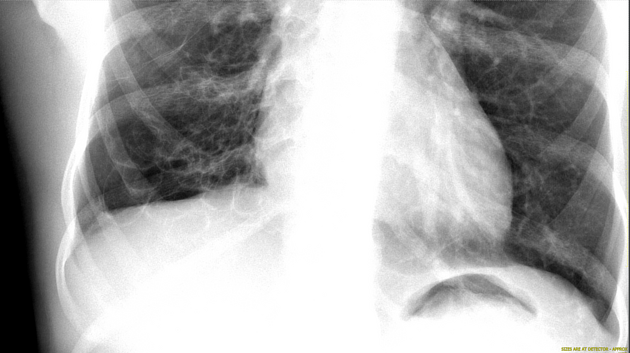
Plain radiograph
Chest x-rays are often abnormal but non-specific. Ring shadows and tram-track opacities represent end-on and en-face dilated bronchi respectively. Air-fluid levels in cystic bronchiectasis may indicate current infection. Peri-bronchovascular fibrosis may obscure the bronchovascular structures 8,9.
CT
CT is diagnostic and may help identify the cause. A number of features are helpful in diagnosing bronchiectasis 8,9:
-
bronchus visualized within 1 cm of the pleural surface 20
especially true of lung adjacent to costal pleura
most helpful sign for early cylindrical change
lack of tapering
-
increased bronchoarterial ratio 9
diameter of a bronchus should measure approximately 0.65-1.0 times that of the adjacent pulmonary artery branch
between 1 and 1.5 may be seen in normal individuals, especially those living at high altitude
greater than 1.5 indicates bronchiectasis
A number of ancillary findings are also recognized:
bronchial wall thickening: normally the wall of bronchus should be less than half the width of the accompanying pulmonary artery branch 25
mucoid impaction 25
Signs described on CT include:
Treatment and prognosis
In general, the treatment of bronchiectasis is medical and involves promoting sputum clearance, using positional physiotherapy, and early and aggressive treatment of pulmonary infections. In some cases, chronic prophylactic administration of antibiotics may be required. In certain etiologies, specific pharmacotherapy may be available (e.g. cystic fibrosis transmembrane regulator (CFTR) modulators in cystic fibrosis).
In cases where bronchiectasis is severe and significant morbidity is present, surgical resection of the affected lobe may be of the benefit provided adequate respiratory reserve exists. In cases where both lungs are extensively involved (e.g. cystic fibrosis), bilateral sequential lung transplantation can be considered 10.
History and etymology
The term bronchiectasis is derived from the Greek words bronckos (βρόγχος) meaning airway/loop and ectasis (έκταση) meaning widening.
Differential diagnosis
Reversible bronchial dilatation can occur, and is relatively common in organizing pneumonia.
Causes of a particular distribution of bronchiectasis
Mimics of bronchiectasis
Conditions that may mimic cystic bronchiectasis include 8:

















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.