Pulmonary metastases refer to distant tumor spread from a variety of primary tumors to the lungs via the blood or lymphatics.
This article primarily describes hematogenous pulmonary metastases while lymphangitic carcinomatosis is discussed separately.
On this page:
Epidemiology
Lung metastases are common. The incidence of synchronous lung metastasis at initial cancer presentation is about 18 per 100,000, noting this figure does not include metachronous metastases (occurring after initial cancer staging) 8. The incidence is slightly higher in males (20 in 100,000) than females (16 in 100,000) 8. The specific epidemiology reflects that of the underlying malignancies (see below).
As malignancies increase in incidence with increasing age, so does the incidence of synchronous pulmonary metastases. Below age 40, the incidence is about 1 in 100,000, while above age 40, the incidence is about 40 in 100,000 8. The peak incidence reaches 116 per 100,000 in patients age 80-84 8.
Clinical presentation
Pulmonary metastases are usually asymptomatic or can present with hemoptysis, dyspnea, and pneumothorax. Symptoms more commonly arise from the primary tumor, extrapulmonary metastates or systemic effects 5.
Pulmonary thrombotic microangiopathy is an exception, causing hypoxemia, pulmonary hypertension, cor pulmonale, rapid decline and death 10. Gastric carcinoma is the most common primary.
Pathology
Tumors spread to the lungs in a variety of ways:
direct invasion from an extrapulmonary tumor
hematogenous capillary embolization and intra-parenchymal growth
intravascular tumor embolus and intravascular growth
tumor microangiopathy (causing pulmonary hypertension and death)
airway spread
lymphatic spread
Etiology
The most common malignancies to present with pulmonary metastases are the following that predominate in middle age to older adults, each occurring with an incidence of greater than 1 in 100,000 8:
lung cancer (most common primary site)
In young men aged 15 to 40, testicular cancer is the most common cause of synchronous lung metastasis 8.
In adolescents aged 10 to 20, bone and soft tissue sarcomas are the major sources in both sexes 8. Under age 10, kidney and soft tissue tumors dominate 8. The most common primaries for pediatric pulmonary metastases are the following histologies:
Alternatively, primaries that most frequently metastasize to lungs (although are much less common) include 1,3:
Primaries that metastasize as endobronchial deposits can include:
Radiographic features
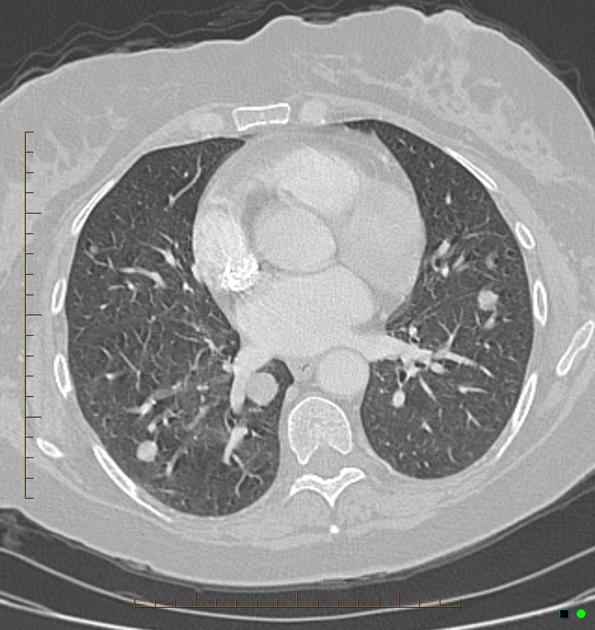
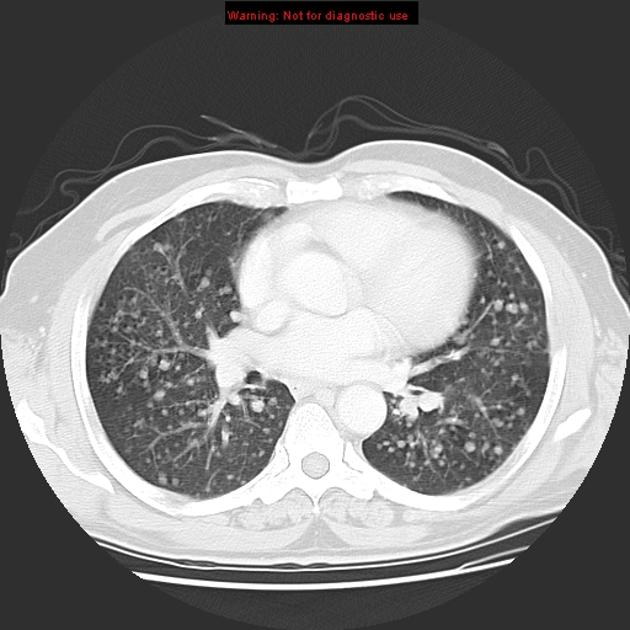
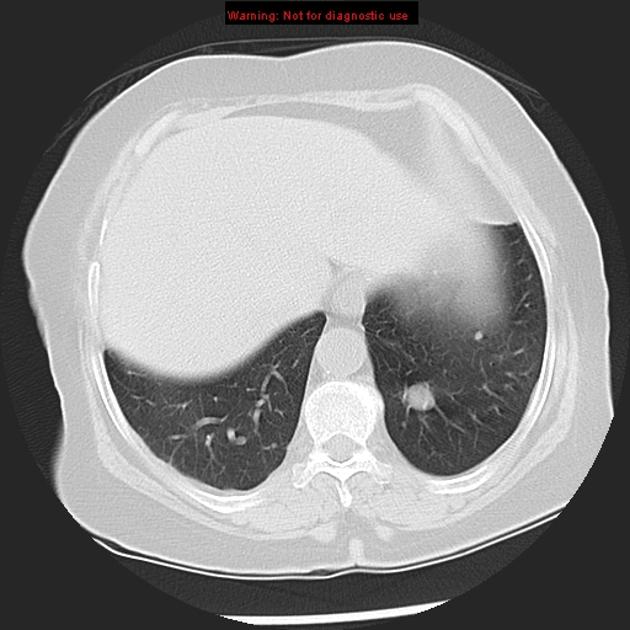
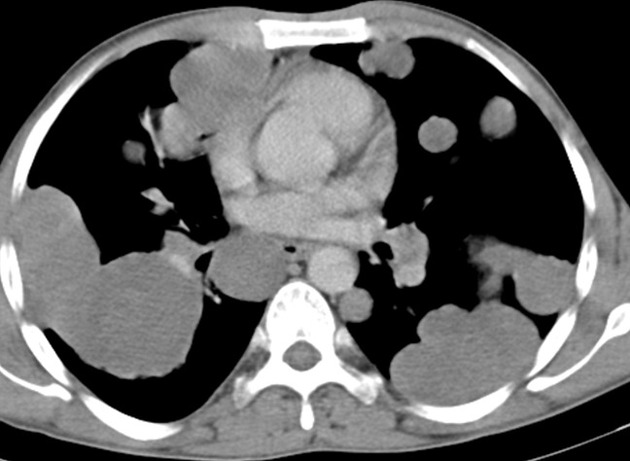
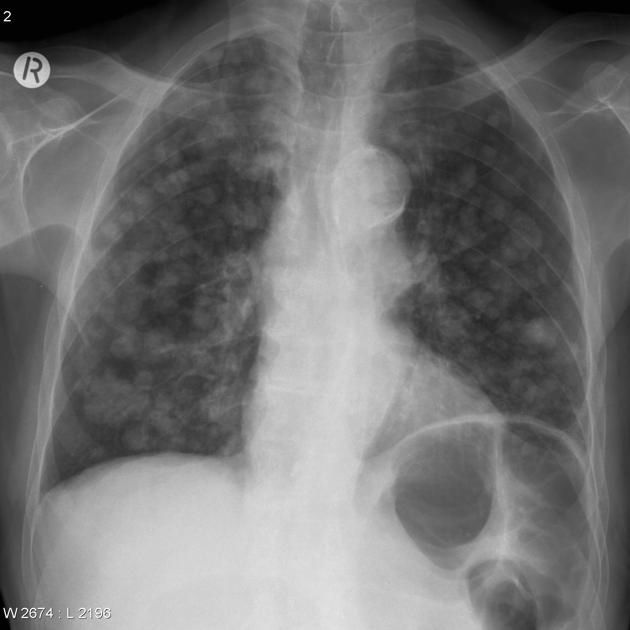
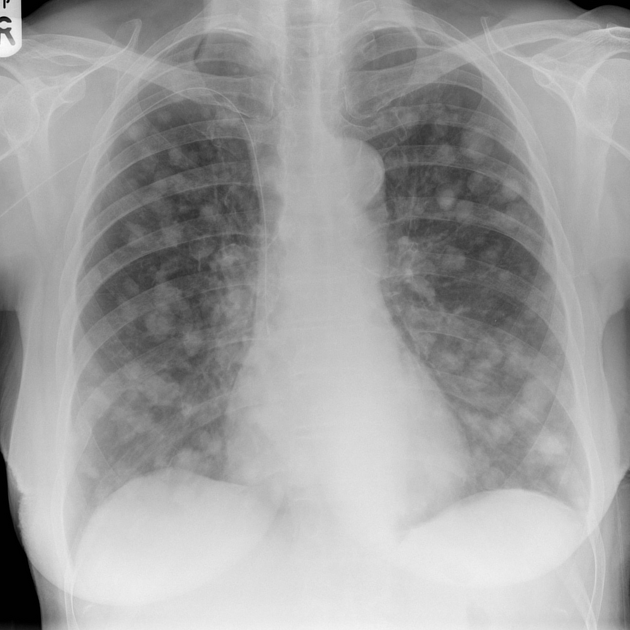
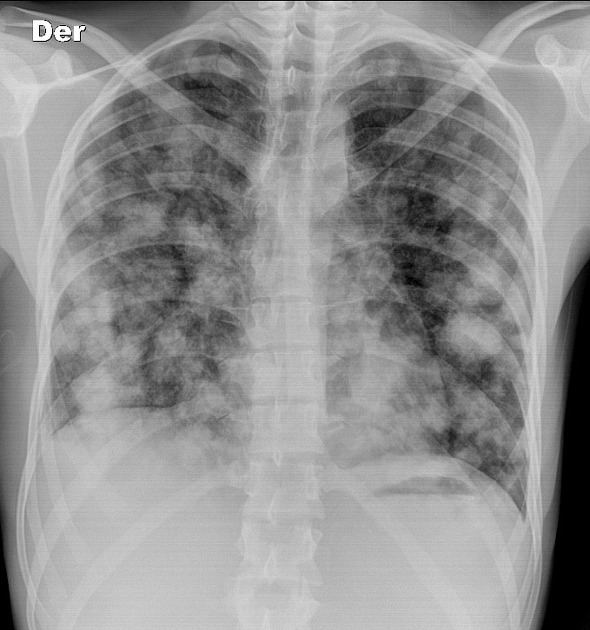
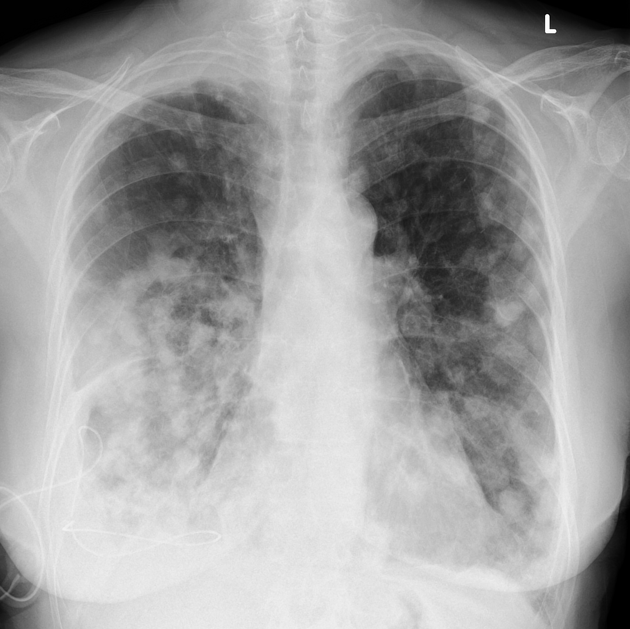
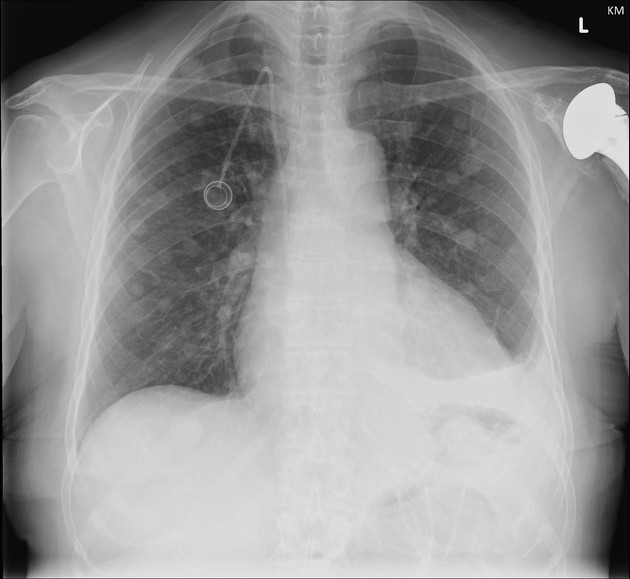
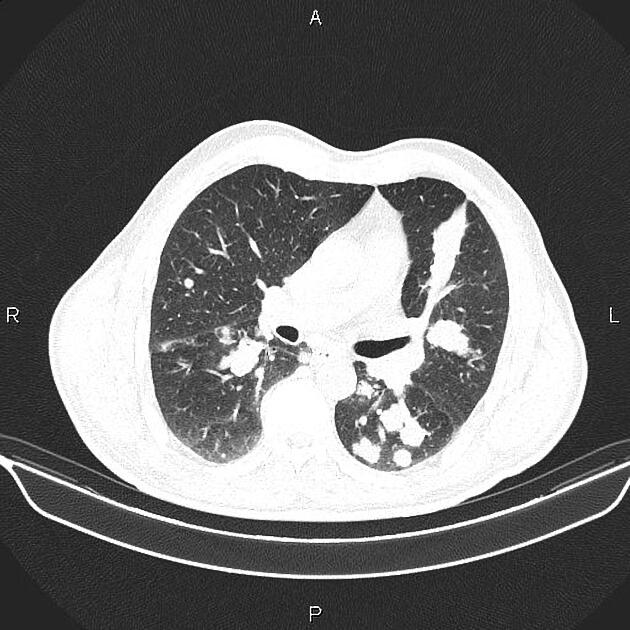
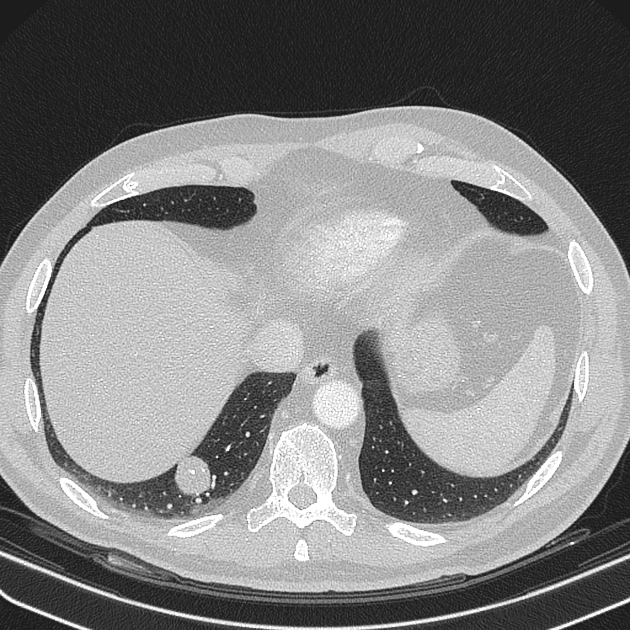
Pulmonary metastases typically appear as multiple, peripheral, rounded nodules scattered throughout both lungs 1. Larger nodules and masses may be termed cannonball metastases. Atypical features include consolidation, cavitation, cystic change, calcification, ossification, hemorrhage, and secondary pneumothorax.
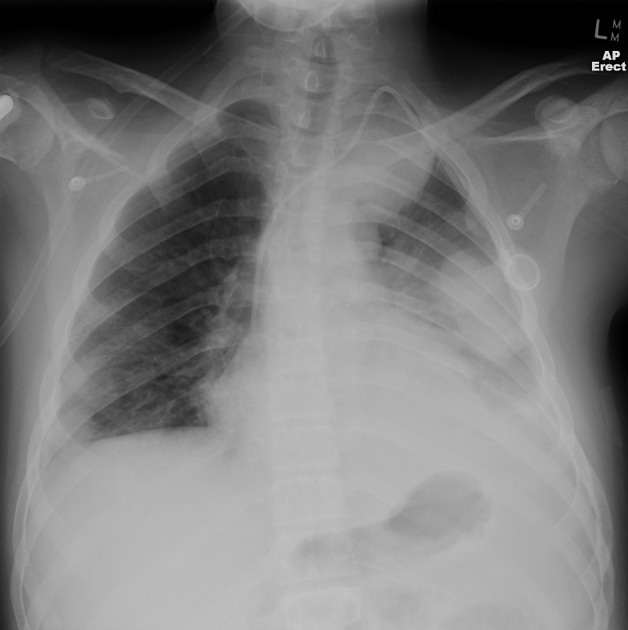
Plain radiograph
Plain films are insensitive, although frequently able to make the diagnosis, as often pulmonary metastases are large and numerous.
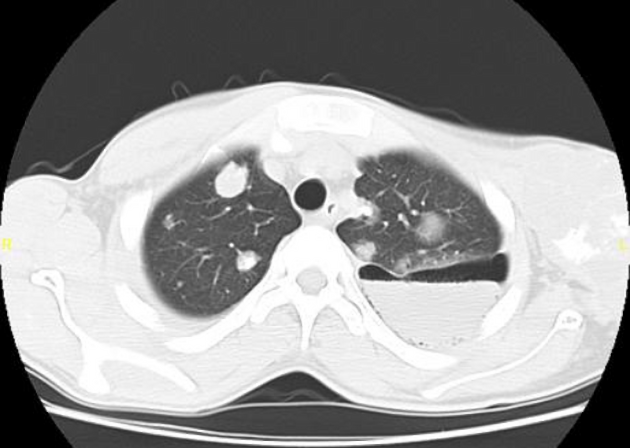
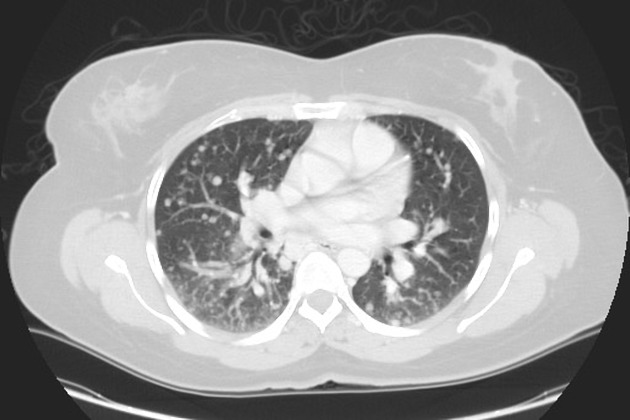
CT
CT is excellent at visualizing pulmonary nodules. Typically, metastases appear of soft tissue attenuation, well circumscribed, rounded lesions, more often in the periphery of the lung. They are usually of variable size, a feature which is of some use in distinguishing them from a granuloma 3.
A prominent pulmonary vessel has frequently been noted heading into a metastasis. This has been termed the feeding vessel sign 4. It is unclear whether this is a true finding or the result of older scanners with thicker slices resulting in volume averaging 4. However, a number of atypical features are commonly encountered.
Some tumors have a predilection for innumerable small metastases (miliary pattern):
Conversely, a pulmonary metastasis may be single. This is most frequently seen in colorectal carcinoma but can be seen with other primary tumors 3:
skeletal sarcoma
adenocarcinomas in general
Adenocarcinoma metastases, rather than displace or destroy adjacent lung parenchyma, may grow in a lepidic fashion (spread along alveolar walls) resulting in pneumonia-like consolidation. Air bronchograms may also be visible 1.
Cavitation is present in ~4% of cases 1. The most common primary is squamous cell carcinoma, most often from the head and neck or from the lung. Other primaries include adenocarcinomas, and sarcomas 1,3.
Calcification, although uncommon and more frequently a feature of benign etiology (e.g. granuloma or hamartoma) is also seen with metastases, particularly those from papillary thyroid carcinoma and adenocarcinomas. Treated metastases, osteosarcomas and chondrosarcomas may also contain calcified densities 1.
A halo of ground-glass opacity representing hemorrhage can be seen, particularly surrounding hemorrhagic pulmonary metastases, such as choriocarcinoma and angiosarcoma 1.
Dual energy CT
Some studies some added capacity in differential intrapulmonary metastases with dual energy CT based on iodine concentration 9.
MRI
Although not used routinely, MRI may be as sensitive in the detection of pulmonary metastases as CT 2,4.
Treatment and prognosis
In general, pulmonary metastases are an ominous finding, indicating poor prognosis. The specific prognosis will, however, depend on the primary tumor.
Complications
Tumors with prominent necrosis located near a pleural surface may result in a pneumothorax. Osteosarcoma is classically described as the pulmonary metastasis that results in pneumothorax. Another cause of pneumothoraces includes cystic or cavitary pulmonary metastases.
Differential diagnosis
The differential depends on the number of nodules/masses and their imaging characteristics.












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.