Williams-Campbell syndrome
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
View Yuranga Weerakkody's current disclosuresAt the time the article was last revised Subhan Iqbal had no financial relationships to ineligible companies to disclose.
View Subhan Iqbal's current disclosures- Williams-Campbell syndrome (WCS)
- Williams-Campbell syndrome
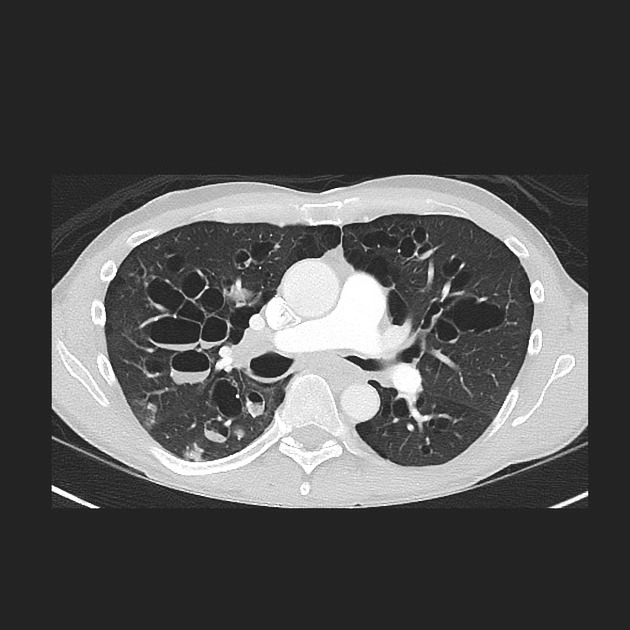
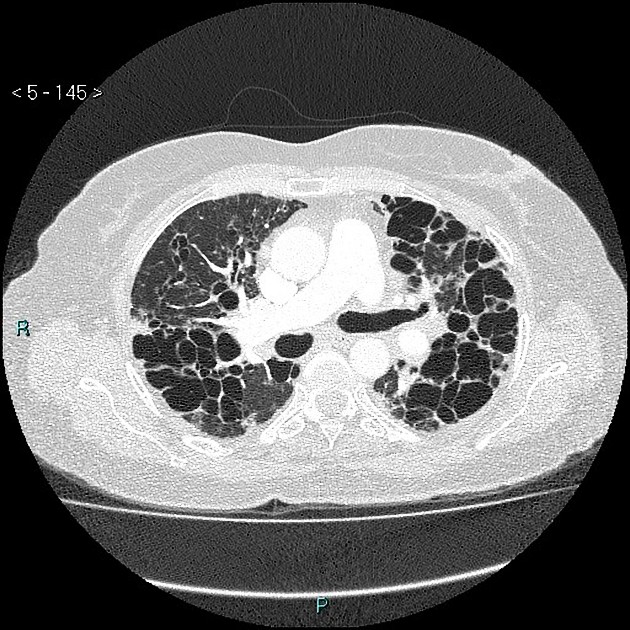
Williams-Campbell syndrome (WCS) is a rare form of congenital cystic bronchiectasis, in which distal bronchial cartilage is defective.
On this page:
Clinical presentation
Williams-Campbell syndrome may present with recurrent pneumonia, wheezing, pulmonary hypertension, barrel-chest deformity, and Harrison sulcus 8,10.
Pathology
It is thought to develop from a deficiency of cartilage formation in the 4th to 6th order sub-segmental bronchi, resulting in distal airways collapse and bronchiectasis 6,7.
Radiographic features
CT
Cystic central bronchiectasis changes, usually symmetric and bilateral, typically involving 4th to 6th order bronchi with preservation of the trachea and main bronchi 2. On expiratory aquisitions, there is characteristic collapse of affected bronchi 9.
History and etymology
The syndrome was first described by Howard Williams and Peter Campbell in 1960 8.
Differential diagnosis
All causes of diffuse and bilateral bronchiectasis including:
References
- 1. McAdams HP, Erasmus J. Chest case of the day. Williams-Campbell syndrome. AJR Am J Roentgenol. 1995;165 (1): 190-1. doi:10.2214/ajr.165.1.7785587 - Pubmed citation
- 2. Marom EM, Goodman PC, McAdams HP. Diffuse abnormalities of the trachea and main bronchi. AJR Am J Roentgenol. 2001;176 (3): 713-7. doi:10.2214/ajr.176.3.1760713 - Pubmed citation
- 3. Webb WR. Radiology of obstructive pulmonary disease. AJR Am J Roentgenol. 1997;169 (3): 637-47. doi:10.2214/ajr.169.3.9275869 - Pubmed citation
- 4. Acar T, Bayraktaroglu S, Ceylan N et-al. Computed tomography findings of tracheobronchial system diseases: a pictorial essay. Jpn J Radiol. 2015;33 (2): 51-8. doi:10.1007/s11604-014-0380-3 - Pubmed citation
- 5. Konoglou M, Porpodis K, Zarogoulidis P et-al. Williams-Campbell syndrome: a case report. Int J Gen Med. 2012;5: 41-4. doi:10.2147/IJGM.S28447 - Free text at pubmed - Pubmed citation
- 6. Noriega Aldave AP, William Saliski D. The Clinical Manifestations, Diagnosis and Management of Williams-Campbell Syndrome. N Am J Med Sci. 2014;6 (9): 429-432. doi:10.4103/1947-2714.141620 - Free text at pubmed - Pubmed citation
- 7. Liu M, Liu YQ, Liu ZH, Liu WY, Liu. Williams-Campbell syndrome complicated with pulmonary hypertension and Type 2 respiratory failure: An adult case report. (2019) The clinical respiratory journal. doi:10.1111/crj.13090 - Pubmed
- 8. WILLIAMS H, CAMPBELL P. Generalized bronchiectasis associated with deficiency of cartilage in the bronchial tree. (1960) Archives of disease in childhood. 35: 182-91. doi:10.1136/adc.35.180.182 - Pubmed
- 9. Ghosh S. Williams-Campbell Syndrome. Radiology. 2021. doi:10.1148/radiol.2021211621
- 10. Liu M, Yuan Q, Zhao H, Wang Y. Williams‐Campbell Syndrome Complicated with Pulmonary Hypertension and Type 2 Respiratory Failure: An Adult Case Report. Clinical Respiratory J. 2019;13(12):795-9. doi:10.1111/crj.13090 - Pubmed
Incoming Links
Related articles: Chest
- imaging techniques[+][+]
-
chest radiograph
- radiography
-
approach
- ABCDE
- ABCDEFGHI
- congenital heart disease
- medical devices in the thorax
- common lines and tubes
- nasogastric tubes
- endotracheal tubes
- central venous catheters
- esophageal temperature probe
- tracheostomy tube
- pleural catheters
- cardiac conduction devices
- prosthetic heart valve
- review areas
-
airspace opacification
- differential diagnoses of airspace opacification
- lobar consolidation
-
atelectasis
- mechanism-based
- morphology-based
- lobar lung collapse
- chest x-ray in the exam setting
- cardiomediastinal contour
- chest radiograph zones
- tracheal air column
- fissures
- normal chest x-ray appearance of the diaphragm
- nipple shadow
-
lines and stripes
- anterior junction line
- posterior junction line
- right paratracheal stripe
- left paratracheal stripe
- posterior tracheal stripe/tracheo-esophageal stripe
- posterior wall of bronchus intermedius
- right paraspinal line
- left paraspinal line
- aortic-pulmonary stripe
- aortopulmonary window
- azygo-esophageal recess
- spaces
- signs
- air bronchogram
- big rib sign
- Chang sign
- Chen sign
- coin lesion
- continuous diaphragm sign
- dense hilum sign
- double contour sign
- egg-on-a-string sign
- extrapleural sign
- finger in glove sign
- flat waist sign
- Fleischner sign
- ginkgo leaf sign
- Golden S sign
- Hampton hump
- haystack sign
- hilum convergence sign
- hilum overlay sign
- Hoffman-Rigler sign
- holly leaf sign
- incomplete border sign
- juxtaphrenic peak sign
- Kirklin sign
- medial stripe sign
- melting ice cube sign
- more black sign
- Naclerio V sign
- Palla sign
- pericardial fat tag sign
- Shmoo sign
- silhouette sign
- snowman sign
- spinnaker sign
- steeple sign
- straight left heart border sign
- third mogul sign
- tram-track sign
- walking man sign
- water bottle sign
- wave sign
- Westermark sign
- HRCT
-
chest radiograph
- airways
- bronchitis[+][+]
- small airways disease
-
bronchiectasis
- broncho-arterial ratio
- related conditions
- cystic fibrosis
- allergic bronchopulmonary aspergillosis
- Williams Campbell syndrome
- congenital tracheobronchomegaly (a.k.a. Mounier Kuhn syndrome)
- primary ciliary dyskinesia
- differentials by distribution[+][+]
- narrowing[+][+]
-
tracheal stenosis
- diffuse tracheal narrowing (differential)
-
bronchial stenosis
- diffuse airway narrowing (differential)
-
tracheal stenosis
- diverticula[+][+]
- pulmonary edema[+][+]
-
interstitial lung disease (ILD)[+][+]
- Anti-Jo-1 antibody-positive interstitial lung disease
- drug-induced interstitial lung disease
-
hypersensitivity pneumonitis
- acute hypersensitivity pneumonitis
- subacute hypersensitivity pneumonitis
- chronic hypersensitivity pneumonitis
- etiology
- bird fancier's lung: pigeon fancier's lung
- farmer's lung
- cheese workers' lung
- bagassosis
- mushroom worker’s lung
- malt worker’s lung
- maple bark disease
- hot tub lung
- wine maker’s lung
- woodsman’s disease
- thatched roof lung
- tobacco grower’s lung
- potato riddler’s lung
- summer-type pneumonitis
- dry rot lung
- machine operator’s lung
- humidifier lung
- shower curtain disease
- furrier’s lung
- miller’s lung
- lycoperdonosis
- saxophone lung
-
idiopathic interstitial pneumonia (mnemonic)
- acute interstitial pneumonia (AIP)
- cryptogenic organizing pneumonia (COP)
- desquamative interstitial pneumonia (DIP)
- non-specific interstitial pneumonia (NSIP)
- idiopathic pleuroparenchymal fibroelastosis
- lymphoid interstitial pneumonia (LIP)
- respiratory bronchiolitis–associated interstitial lung disease (RB-ILD)
- usual interstitial pneumonia / idiopathic pulmonary fibrosis (UIP/IPF)
-
pneumoconioses
- fibrotic
- non-fibrotic
-
lung cancer[+][+]
-
non-small-cell lung cancer
-
adenocarcinoma
- pre-invasive tumors
- minimally invasive tumors
- invasive tumors
- variants of invasive carcinoma
- described imaging features
- adenosquamous carcinoma
- large cell carcinoma
- primary sarcomatoid carcinoma of the lung
- squamous cell carcinoma
- salivary gland-type tumors
-
adenocarcinoma
- pulmonary neuroendocrine tumors
- preinvasive lesions
-
lung cancer invasion patterns
- tumor spread through air spaces (STAS)
- presence of non-lepidic patterns such as acinar, papillary, solid, or micropapillary
- myofibroblastic stroma associated with invasive tumor cells
- pleural invasion
- vascular invasion
- tumors by location
- benign neoplasms
- pulmonary metastases
- lung cancer screening
- lung cancer staging
-
non-small-cell lung cancer





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.